There are no products in your shopping cart.
YOU and Your Brain Injury: Concussions in Young Athletes Leading to Health Care Reform
After January 1, 2012, student athletes in Colorado sustaining a "head injury" (as they are commonly called, but ultimately is a 'brain injury' and we should be using THAT word to show the importance every time it's uttered) will finally have a fighting chance of a "concussion" (which is a physics word that the health industry adopoted, again, it undermines the importance of the BRAIN is INJURED) occurring during school activities not impacting the rest of their lives. Or, in the worst case, ending their young lives due to 'second impact syndrome' (SIS). It begs the question 'where are our priorities?' I hope parents and young people all think this through. As in really give it some time and thought.
There is a fascinating story about how this came to be, with many "players" over seven years making an impact on changing how brain injuries are viewed, handled and recovered from. Through students and their families/friends ("framilies" I affectionately call them) becoming more aware about brain injury and all things related, it will extent out to the community and eventually have a positive impact on older people as well.
This new law is requiring the "student/framily unit" to collaborate to be the YOU in the middle of the team, and realistically, they might need an advisor there with them. I realize I have a big different background than some occupational therapists today, and that is why I don't operate as an OTR but as a 'functional advisor and consultant'.
In this series, I hope to provide a base of information for those who have young brains they're caring about protecting or healing/restoring to wellness or as close as can be to it, as that brain goes with YOU (the young person) for the rest of your life and YOU remain "chronically well" or end up in "chronic illness" (and everyone is somewhere along that continuum). Related to brain injuries, there are other topics in this forum so please navigate with the links above this topic's title and go 'up' to the forum and see the list.
I'll also set people up for further exploration of various information based upon the brains I pick of the experts I know who specialize in things related to the brain. I also am providing links and utilizing highlights of some exceptionally well done stories I've found related to how Jake Snakenberg's school psychologist has changed the course of how head injury is handled in Colorado.
The History of The Jake Snakenberg Law
Initially responsible for us to appreciate in all this, and most importantly, is a young man from Aurora, Colorado named Jake Snakenberg, whose life ended in 2004 at age 15 related to head injuries sustained from playing football. Next, the school psychologist in his school at the time, Dr. Karen McAvoy, along with the many since, who have collaborated to create new organizations and processes, clearly progressing how we are handing head injury related to school-related incidents. She now heads a nonprofit which focuses on head injury in young people. I provide more information about this story and links to my resources for writing this piece, below, and encourage those who are particularly interested, to follow and enjoy the details I've not included in this piece; as I say, it's an inspiring read, and for me, raised a lot of questions and ideas. For one thing, there is a quote in a big newspaper story about it by a physician who says that there's nothing you can do for the brain but let time heal it. That didn't sound right to me, from my perspective about medicine.
By shining the light on the effects of head injury, even minor ones also known as 'concussions', I foresee The Jake Snakenberg Law to lead to the 'hammer of health care' to swing in new directions, eventually impacting in a positive way the health of Colorado's residents in a positive manner. I forsee this to initially extend to other young people in schools injured in playground mishaps, slips/falls, and violence-related incidents.
Due to the parents and family/friends ("framily") becoming educated about head injury from their children, the entire community will have much more awareness about brain injury in the short and long-term, much the way texting on cellular telephones has evolved in awareness as an issue for wellness/safety. Medical providers are being educated about the law and are involved as key players on the team deciding if and when and how a student can go back to not only physical activity at school but cognitive/thinking activities. Hopefully this will bring a long-overdue increase in interest in continuing education when the providers are making choices on where to put their continuing education resources of time, energy, and money. And I will work to provide quality information at Lumigrate.com for those who look to us for education from our perspective, which is an increasingly popularly held one, even among conventional physicians/medicine!
The other exciting element, from my standpoint, is it has been wisely designed to be 'collaborative': the student and their adult teammates (typical parents), the school personnel, and the medical provider have to work together. This will go far with 'reforming' health care. The Lumigrate You Model, which has been our cornerstone since the beginning, lends itself well to this situation. Here is how the Lumigrate You Model looks for the medical consumer when using a collaborative approach and integrative medicine, which addresses body, mind and spirit. 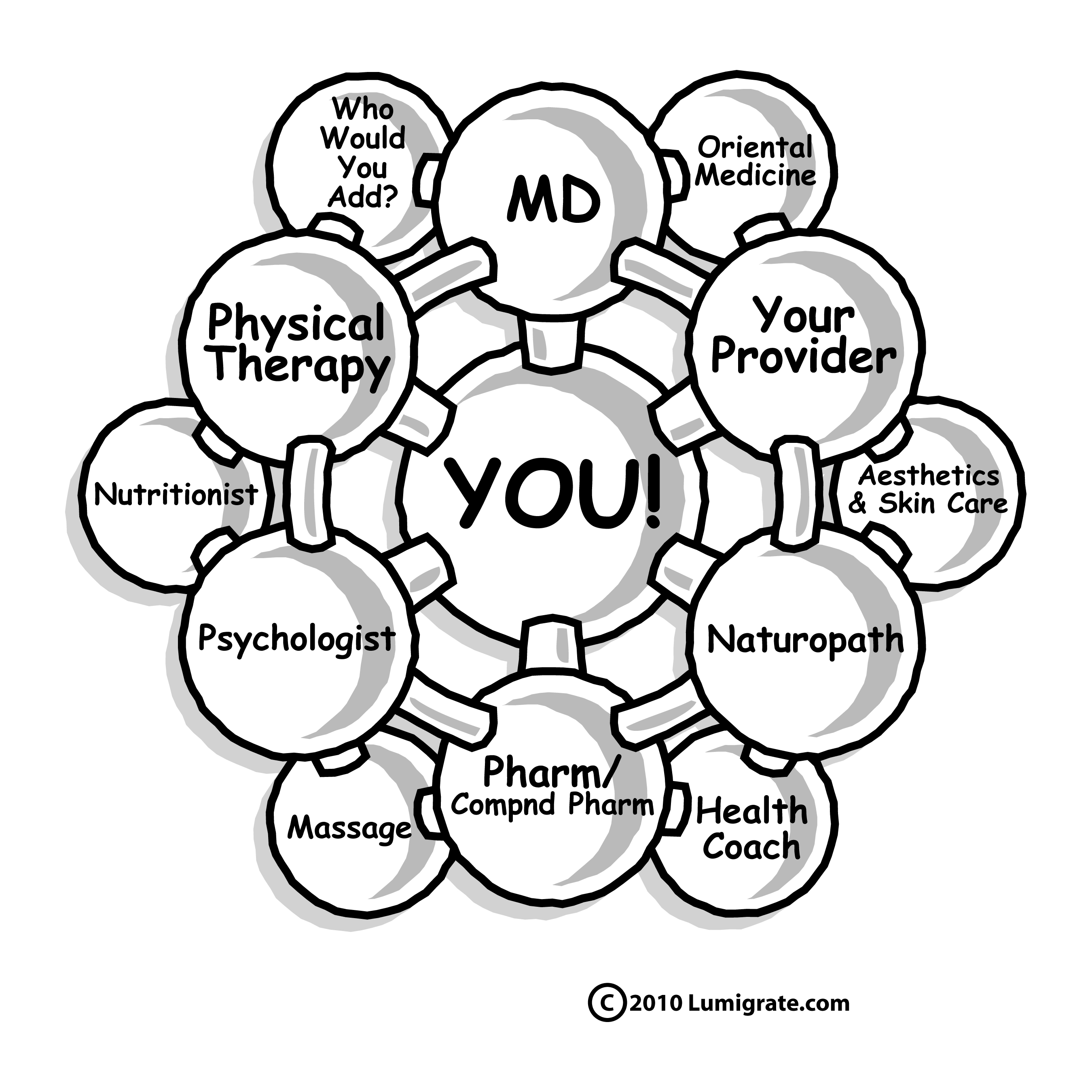 Integrating the Jake Snakenberg Law with the Medical System; Difficulties?
Integrating the Jake Snakenberg Law with the Medical System; Difficulties?
To ease the difficulties of implementing this new law, specialists in function and problem solving could partner with the student's 'team' of health care/school professionals post brain injury from three ways:
1) the "framily" utilizing an independent consultant to act on their behalf as an advocate, liaison, advisor and detective to 'bird-dog' the information needed and consolidate it,
2) the schools utilizing existing or additional occupational therapists and other qualified para-professionals to assist the school personnel with this added responsibility placed upon them and
3) the medical providers/clinics bringing on additional qualified staff since they are, by law, tasked with assessing where the head injury is at related to healing, which requires doing testing and knowing what the baseline/before head injury cognitive function was.
Information to be taken into account includes grades in various subjects, standardized tests which can be compared with the results of the post-concussion cognitive testing, verbal report, etc. Depending upon the severity of the injury and how the student responds after it, there are going to be a LOT of variations to consider.
This kind of decision-making is similar but different than what most physicians have been doing their careers, and this is going to be a cumbersome process that people essentially get thrown into instantly with a 'ring of the bell'/(concussion). Technology and the short time allowed by insurances between provider and patient have resulted in physicians honing their skills and interpreting a lab result and offering a solution from there. So many people have stories of missed diagnoses or mis-diagnosis as a result. It's rampant and I know few physicians who don't have the best intentions at heart, or they used to before they became so overwhelmed by today's environment.
Over a decade ago, for two years I worked with 15-20 year old first-time drivers who had difficulties passing the driving program where I was the resident rehabilitation specialist (program director), and it took me the better part of half an hour to get a good oral history from the framily and student to find out what might be the underlying problem and then go about solving it.
I'd previously been certified in the Assessment of Motor and Process Skills, a standardized tool for occupational therapists who are called upon in geriatrics to determine if a person is safe to stay in their home or assisted living with the support they have, or whether it's recommended to have them go to another situation with more (or less) assistance. These are the types of skills that are going to be required in making the best decisions about returning students to thinking or playing at school.
Call it what it is: "Brain Injury" vs. "Concussion"
I believe it is best to not call them 'concussions' anymore except parenthetically or in titles and search word strings, since that's what many people have historically called them. Brain injury is brain injury, the is a continuum from mild to severe. Calling it 'concussion' can perpetuate that word usage and times when a 'concussion' was something we just got up from and kept going; we now know that's not the right thing to do.
"Seeing stars ... and we all get them at some point and it all resolves on it's own, no big deal". I'm adamant about how big a deal it is, and I believe there are many health and learning problems in adults and younger people which have been caused by a deficiency of information in the public and medical providers' 'fund of knowledge'. "Brain injury" shifts the conversation to a different level, and I think it's the level that is best for people to really unplug from what they were thinking they were going to be doing right now and shifting it to focusing on the injury and healing.
It is confusing to people to have them called "head injuries" because then it is though there has to be some outward sign on the head/cranium. People may or may not have something sore or visually noticeable, and then the BRAIN, which is really the most important thing inside our bodies, get overlooked. They're brain injuries, from "mild" to "traumatic" (TBI).
From my research recently on this and my years of experience as an OT since 1996 and life-long experience having been born with a brain injury that went under/un/mis-diagnosed for over three decades, the overall medical community is really not very well versed in brain injuries and the strategies available afterwards to remediate them and improve outcomes for the person who sustained one. So I am very concerned about this and am working to build additional information on Lumigrate to address this gap, for those who come to Lumigrate. Naturally, I refer people to it when I am working with them as clients in the consultation aspect of my business.
The Specialists Who Come Into Play After Brain Injury When Things Don't Completely Resolve
I find that many professionals are unaware of the various specialties which are very effective and proven to be beneficial post head injury and want to see people, whether younger or older, know about them at the least and, should they desire, be able to obtain them. I want to suggest that providers and the public realize that the commonality in our frustrations with the medical system is we all feel overwhelmed, wish we had more time to learn, and wish we had more time to spend together in our visits. Medical offices are extremely expensive to run, the overhead is staggering: I should know, I was run out of being in insurance-based occupational therapy because of it!
One solution is to utilize professionals who cost less, and all medical offices have to do that today, but I believe many don't consider outsourcing to qualified providers such as occupational therapists for things that would be completely in their realm of expertise potentially. The think 'nurse'. But nurses don't typically have much training about the brain and function.
With the difficulty presented by the term 'occupational therapist' not being widely understood, the public/consumer/patient might have misconceptions about inviting and including occupational therapists to be on their teams. So perhaps give them a more descriptive title.
Other disciplines don't refer to it frequently enough either; there actually is a bit of discrimination by the PT community against OTs, I'm sorry to say. I've seen it over and over; there are 'OT jokes' like 'blond jokes' or 'lawyer jokes'. I am rarely around a mix of PT/OT anymore but even recently I was at a meeting of health care providers and there was one other OTR present who offered to be part of a demonstration and things were not going completely smoothly -- part of it was the presenter's transmission and the other part was the OTs receiving. I was sitting next to a PT and could literally feel 'the 600 pound elephant in the room', so to speak. It's like I got the telepathy somehow that they were about to make fun of OTs as a category, and JUST as I said 'oh, this is where someone could make an OT joke' the PTs mouth moved and out came the derogatory 'OT slam'. In my health education training prior to becoming an OT, it was drilled into us that you never make a joke about something that is at the expense of a category of people or an individual.
Again, I have universally found the medical world to be one of the most difficult there is to navigate in; 'they eat their own' as I say. It is full of pressures, and I have a great deal of sympathy for the medical offices and providers this law is going to tax: I can 'commiserate"! When I think about the burden of an average of 10 students/team/school/year on the doctors/providers who are already inundated with insurance-based paperwork and trying to communicate with other providers and keep up with it all, I have concerns for all involved.
At the end of the day, my concern and loyalties have ALWAYS been with the patients getting what they should get from giving a professional their time, energy and money/insurance resources. Too often today we hear of a person going to several or more providers without getting anywhere.
Oprah's first show of the new year in 2009, when Lumigrate had recorded a video about hypothyroidism in the fall which was being edited for the new website which launched in March, was about how she had a viewer get ahold of her to say she saw the goiter on her throat; Oprah had been to a handfull of doctors about symptoms that were consistent with thyroid so she asked the sixth one 'have you tested my thyroid' and he looked and ......... none of them had! These stories are everywhere today, and that is why I created Lumigrate, it truly comes down to the consumers looking and listening around until they find something to perhaps take to their provider, the way Oprah did in the earlier example, though in that case it was someone reaching out to her. My thyroid problem was seen by my massage therapist a week after I had been to my specialist who was working with me about low energy and insomnia .. and he had not laid hands on my thyroid nor done the necessary labwork to tease the problem out! Martine Ehrenclou's book we include heavily at Lumigrate, The Take-Charge Patient begins with the story of her going to over 10 providers about horrible abdominal pain and she so brilliantly waits to the end to reveal she had several invasive procedures to the abdominal area, so WE were baffled not being suspicious of herniation. It's just unbelievable one let alone handfulls could miss it! She was doing online research about someone elses medical issues when she came upon information which matched several of her symptoms.
My point is not to beat up the providers, we're already beat up enough overall just from showing up to work each day, but to underscore the importance of YOU taking the time to read about brain injury and what can come from it, so you'll know what you can do about it for someone you know or for yourself, perhaps!
Patients are why we 'do what we do', most people weren't trying to get rich when they put themselves through tons of education -- there are much easier ways to get rich than become a medical provider. All of us have gone to a lot of expense of time, energy and money resources to become providers and be in business for those of use who have ventured out as owners. It frustrates us when we go home at the end of the day and don't feel we've done our best or there's something we might have done wrong. And in my opinion, asking the type of providers tasked in the law with doing what they're going to have to do, I generally fear for the provider and the student/patient and everyone in between.
To my knowledge currently, medical offices don't have pathways in existance with the various schools to get the information, so it seems very inefficient to have each medical office setting all that up. They already have to have that for all the other medical providers, pharmacies and insurance companies, so this is adding another big component to their already overfull plates. However, I commend them in taking on all they do and realize there is an exodus of providers for these reasons. "I can't take it anymore" is being said over and over, not just in medicine, a friend who is a public elementary teacher just said it to me as well. Colorado receives the least amount of funding per student, on average, of all 50 states! So I commend the people who created this movement from a public school tragedy and are creating much OVERDUE change. The medical industry meets the educational industry in this situation and it just has 'difficulties' written all over it to me, I am sorry to say. Again, I'm only reporting on things here as I see them, and offering the solutions I see as opportunities to pick up where any problems leave off! And I universally wish there are no problems but if so, please read on and at other areas of this forum or overall at Lumigrate (Search on keywords).
Theories About Head Injury Treatment and Recovery
I'm proving the links, below, to the two Internet resources I found most helpful in learning more about The Jake Snakenberg Law and they're both excellent and I suggest you follow and read. I bring into this piece the major portions to quote that I feel apply here. In talking with providers over the years and currently, as is reflected in The Denver Post article I link out to later, there's a common belief among medical providers that 'time heals the wounds of head injury'.
I disagree with this, as do the providers at Lumigrate that I have talked to about brain injury. Time IS a factor but it is secondary to other things; primary is what we drink (or not) , breathe in (or not), eat (or not), stress about (or not). This creates the environment in our body which affects the body/brain as time goes by, which translates into healing (more or less/not).
"How we think" -- our 'mind' -- has an increasingly proven affect on the body, known as the mind/body connection. Our spirituality (or not) affects our body/mind system as well and is embraced in 'integrative medicine', which is based on integrating providers related to body/mind/spirit. What about restful, healing sleep? Much has to do in the body with the removal of cellular 'waste' as well, all of which is affected by what you put into the body and how you treat the mind and spirit.
If two identical brains get identical injuries and one person goes home and has pure water to drink and the other drinks 'energy drinks' full of sugar and caffeine and artificial coloring agents, will the brains heal the same? NO WAY, so it's NOT 'time'.
What about the effects of progesterone, which is used in the treatment of significant brain injuries at some ERs .. is there some application for young people related to head injury? Look around Lumigrate for this type of information, in this forum and elsewhere if you're interested. Progesterone affects the GABA/calming neurotransmitter of the brain and therefore it has an effect on people with brain injury, fibromyalgia, and even seizure disorder!
Details of the Jake Snakengerg Law and Western Colorado's Organized Approach using ImPACT Testing
The Jake Snakenberg Law relates to return to school performance after concussion/traumatic brain injury and goes into effect in Colorado on January 1, 2012. This includes not only physical tasks but cognitive/thinking performance. When you are immersed in education and promotion of mind/body/spirit medicine like I am with Lumigrate, it is GRATE that this law and the processes it outlines addresses the mind/body aspect of head injury. From my vantage point, the solutions to head injury come from not just looking at the head and the "obvious" related to not getting another hit to the head when the brain is still healing from the first one, but the relationship of the whole of person's body, mind and spirit related to the injury.
Treatment for head injury in the United States (and in Colorado) Varies Greatly
Brains aren't like bones, where it's either broken or it's not; there is a wide variety of types and extent of injury. I cannot tell you how many times my patients and clients have told me they had some sort of incident where you'd suspect brain injury and when they were at the ER there was a test done of some sort on the brain which showed there was no injury, so therefore there was no brain injury suspected. Yet they clearly had symptoms that went overlooked and untreated, with ongoing symptoms they suspected was from the incident. I'm not a physician, I cannot 'diagnose' things, but since I get to have an hour with a patient not just 10 minutes, I could start putting things together and have been instrumental in many people being properly diagnosed.
Once, a client had been misdiagnosed and treated with an arsenal of medications which, when the physicians collaborated to remove, lead to a 'miracle' of an improved / 'normal' brain on imaging studies. The person's behavior was not normal but since the scan showed it looked normal they couldn't figure out what to diagnose and the legal system could no longer continue to intervene and order medical guardian and lawyer. Again, doctors today have not developed and have lost their clinical reasoning skills so frequently that it sets the patient up for failure all too often. Teams which think 'big picture' see that paying a bit for my time to intervene can save them in the long run.
We've had a lot of dramatic examples recently publicized in the news, from Congresswoman Gabrielle/"Gabby" Giffords, to the thousands of military veterans and others from war-torn areas who are now living with the "the repercussion of concussion". And the public and many providers tend to then think 'that's the bar' where you call it a head injury, rather than thinking the fall that lead to feeling tired after for a while was ALSO a brain injury. A mild one, but it was an injury to the brain.
Brain injury treatment in some communities includes treating with progesterone in the ER through IV; there are progesterone receptors on all cells of the body and when you think about it, there are nerves throughout the whole body (which obviously have cells). There are many opinions about this and MANY other things today with the growing variety of providers, beliefs and information the public is demanding and supporting.
This is where I refer you back to look at The Lumigrate YOU Model, because increasingly the public is responding to/demanding this to be the treatment model and in schools the STUDENT'S PARTICIPATION AND SENSE OF SELF EFFICACY is the key from the very second a brain injury occurs. If they don't accurately know the many repercussions of brain injury and treatment and respect what can happen if they don't stop activity immediately, they might live to regret it. My concern is this law is so geared to the FEW cases where someone dies and not focusing on the MUCH MORE COMMON long term effects of brain injury.
If someone told me "there are millions of brain injuries a year, and 3-4 a year die of second impact syndrome", I doubt even as an adult I'd stop playing! BUT, if I knew that it could affect my chances of ALL the things kids look forward to in life (such as working and having money when they grow up), they have a better chance of handling it correctly from the first impact/head injury. I was the kind of kid that if I knew about the long-term effects we know of today related to repetitive brain injury such as in football, I'd have said 'I'm not playing that sport, let me find another one'. That's really 'all I ask' for starters, is that Lumigrate and I might reach students so they can decide to learn more, what sports to play or not, and certainly what to do if they get a brain injury. Again, please do not minimize it by calling it a 'concussion' it is a 'brain injury'.
Information on Lumigrate Re: Fibromyalgia and Chronic Fatigue Applies to Head Injury
Many of the people who initially followed Lumigrate as a resource for progressive health information did so because of my relatively good recovery at the time from a condition known to be fairly devastating, fibromyalgia. That recovery has much to do with things that I didn't obtain from insurance-based medicine, which does not support nutrition advisement, supplementation, nor the supplementation of biologically identical hormones.
I know first-hand what happens when you only use the allopathic providers and insurances: I did that for a number of years and my health spiraled down to something I wouldn't wish for anyone to experience. Most of the time when I say in conversation to the public that I have fibromyalgia, people lately typically know someone who has it and they know it's something 'really bad' and some seem surprised as they don't think of someone who has it being as active as I am. I've had this relative success, thankfully, because of my using a mixture of insurance-based allopaths in the past and other providers, tests, and treatments that insurance doesn't pay for. I also have invested in what I drink and eat differently than the average American or how I would have otherwise and believe whole-heartedly that my health and therefore life have benefitted from it.
I therefore want to see the young people who get head injuries also have information about things that are not only coming from the school and allopathic communities which are at the crux of this law and new process. And in the long run it will save money, just as my investing money into things others don't support has saved money on my health care. Naturally, for a new system like this to go into effect, it has to be set up on what ALL students have the ability to obtain related to medical providers issuing the required test and yielding a decision about how and when to return to motor and process tasks at school (and otherwise, presumably, but the law doesn't dictate what goes on outside of school). Schools are mandated to provide treatment for anything they tease out and label as a 'problem' in public schools. Today, with increasing variability related to insurance (or not) for diagnosing and treating things, there's been a drastic increase in providers being sought out who are outside of the insurance-based 'loop', and much of this has to do with they are less expensive.
Naturally, the allopathic providers and schools offer us much that is of benefit, but we can't ask them to offer information on things that are outside of their area of strength and expertise. "It takes a village to raise a child" and it takes an INTEGRATIVE team collaborating about the body, mind and spirit of a person whose brain has been injured to have ultimate healing and the best chance of full recovery. There will be a great deal of variability for students, unfortunately, dependent upon their payor sources and those sources beliefs and support of those beliefs. And that is up to the student/framily unit to determine and move forward with.
In my case from my past, a patient was referred to me and when I pulled all the specialists documents together I recommended something and educated about the intervention. The patient and framily checked into it, the patient was well off financially but the framily were leaders in the established allopathic philosophy and guided the patient to pass on the intervention I was requiring to proceed working with me for driving rehab. I made it clear that I was available in the future if they changed their minds. After a competitor passed the patient with some restrictions on hours/light/dark for driving and using adaptive mirrors, there were two incidents in slow situations (thankfully) with the left-neglect problem and they then sought out the treatment I'd originally suggested. A decade has passed with no further incident and has included city, highway, and 'cross' state and Continental Divide driving, which most who drive the route agree it's a challenging drive. So it's sometimes a long process of trial and error, but it starts with identifying the problem and education about options.
The "Occupation of Health Care" and The Lumigrate You Model
From my vantage point from obtaining a degree in occupational therapy in 1996, whose career has more recently focused on education of professionals and the public related to what I call "the occupation of health care", the occupational therapist has much to provide when it comes to the young athletes and others in school-related incidents which are being captured in this new law. In the last handfull of years, I have focused, with great success for those who embrace the concept, on getting the public/patients/consumers educated about what is important to them and putting themselves as the "YOU" in the middle of the health care team and surrounding that "YOU" with the appropriate experts to consult with for advisement on their health. They, in essence, lead the medical providers and the medical community and system to change and adapt; any provider doesn't sincerely embrace this concept doesn't last on my medical team.
It isn't a pain-free transition, but in the end it puts the responsibility of my body/mind/spiritual health and wellness on me, the patient/consumer/client. When you pause and think about the repercussions of that on each person and on the medical system, which includes the legal system related to litigation and the mounting friction between providers and consumers/patients, it is an enormous paradigm shift which greatly affects costs and outcomes. Whether it's the 'terrible two's and three's' or the tween/teen years or the years in between, giving youth the responsibilities they are up to taking on, with support from the adults and 'framily' in their life, yields the best results.
I therefore see this as a huge opportunity to make significant change in the health of many people as well as the 'system' of our interaction with health care providers, particularly if we include them appropriately in the process. Young people who are known to have a head injury in school-related events are going to now have a process initiated which requires collaboration between them, their parents and I prefer to use the word 'framily' to capture today's different social structures in the home and community, and the medical system.
What Type of Medical Providers and How They Medically Clear Student for Return to Play/Think
The medical provider responsible for determining when the head injury is resolved enough to allow for return to limited or full thinking/mental and physical activities has the burden of responsibility legally to be making a good assessment; if they clear someone who in fact is not healed and there's another head injury, the patient might die. This law only holds the medical provider responsible if a second impact syndrome occurs, but it opens the doorway for other legal action related to other long-term effects of head injury. MDs, DOs, NPs, PAs, PhD Psychologists with concussion training are listed in the law to give the medical clearance.
It's not really different than any time a provider makes a recommendation to take a medication or not, have a surgery or not, etc., but there are some challenging complexities related to compiling the information (which is more an administrative time demand) and then cyphering that and determining how the person's doing compared to before the injury which are difficult for the typical primary care physicians and related providers who are tasked with this responsibility. To me, this is something that takes a lot of specific experience and expertise, and I believe occupational therapists can be a very good tool for assisting the responsible providers.
When I read about the specific case of Jake Snakenberg's last week of life, where his symptoms were acknowledged and reported by him to be tingling hands, I don't only wonder "what if the initial head injury had been recognized by him, his family and coaches", but also "if a young person in 2012 has tingling in the hands as he did, and the schools are now teaching all involved to know the signs and symptoms to look for and then sending them to medical providers within 24 to 72 hours for assessment, will the medical providers consulted know what interventions to recommend?" I wonder "if he'd not had a second impact but also hadn't had any treatment, what would his health and learning/school wellness have been like?"
I have a former patient who had multiple 'concussions'/head injuries in his youth and then in his young adulthood had another head injury related to a motorized vehicle crash and the initial medical team and the patient and framily hadn't had enough education related to 'concussion' back then, helping me form my opinion about calling them 'head injury' instead. That patient started with treatments for the body/brain and mind paid for by insurances, then outside of insurances, and after exhausting all known possible treatments turned to more emphasis on spirituality there was a big improvement which came at that point. Naturally, it appears that it was 'time', but from my vantage point it was the interventions for body/mind/spirit which occurred over time which finally resulted in a return to work and being considered 'within normal limits' for activity (which is generally considered 80% of ideal for age and background when looking at chronic fatigue.)
History and Resources about Jake Snakenberg Law
I am finding the story behind the Jake Snakenberg Law an intriguing one, not only because of the aspect of something good for many young people coming out of the circumstances of one 'untimely and unfortunate' death in 2004, but because I forsee the process of school and medical professionals collaborating together with each other and the student and his/her family leading to more changes for ALL in this country related to medical care. Where small grooves are created, they are deepened by more that follow in the tracks of the previous, whether that be wearing a pathway, creating a new waterway, or changing how we obtain our medical care.
The youth who are handled for head injuries are going to be like a bulldozer for this process by the time they are parents with children following in their footsteps in school athletics. At least I hope I am seeing this correctly, for their sake, as the current health care system is the number one challenge for the majority of people in the United States no matter what their income and education. I find it what we all have in common and the greatest place to focus on change. Hence my anticipation about where things change in 2012 with this new law and process.
The law is inspired by an infrequent but serious condition which has occurred in the United States about 30-40x/decade in the past, called "second impact syndrome", which can occur when there is a second concussion/head (brain) injury sustained before symptoms have cleared from an initial injury to the brain, causing swelling, death or severe disability. Naturally, we wouldn't want this to happen to any one of our young athletes, so I believe this is big and good step forward for the people of Colorado -- and beyond.
More importantly, it is casting a light on head injury from things 'we can all relate to'. We've had a lot of exposure recently to the head injuries sustained by our military with the types of weapons being used increasingly in combat, but unless you've been in Hummer driving down main street and had a bomb detonate nearby, you might not 'relate' to having had a head injury in the past. But with this, everyone might stop and say "I had a head injury when I was younger, I wonder if that has anything to do with what I'm experiencing today".
As a person with a history of complex medical issues, the first step, as with anything, is awareness and education. Then the next step is to take action; as Nike's famous slogan says "Just Do It". I prefer to call it "patient proactivity" and believe it relates to feelings of self-efficacy. That applies here particularly since we're talking about athletic-related injuries in this piece, which can have lasting and insideous but profound affects on people's lives. (For those who wish to read more about the details of how I came full circle on this, more can be found at the following link related to as much as I have come to understand and can relate related to my case: LINK HERE
For every instance where someone dies as a result of concussions not properly recognized and treated, there are uncountable numbers of others who end up with life altering changes. Sometimes these are long-term effects which cause significant change in function and affect a person's life, at great expense to them as people and to all who are affected by the finances related to that person. That ends up having an impact on all of us in the society, but mostly devastates the life of the person and potentially their family.
I have seen it said that the average student athlete's costs for athletic competition is $10,000; I hope when an unfortunate injury occurs the treatment plan for these students and their supervising adults includes education about the positives and negatives about the things which affect the body. Unfortunately, health care costs have not historically been something Americans think of as being one of 'their' responsibilities, but that is changing and many are now seeing the wisdom in being proactive and shifting resources to do things preventively. But inevitably, there's a time/money/energy equation many are constantly challenged by.
The Effects of Nutrition on Youth/Injuries
THE PROCESS MY LOCAL SCHOOL DISTRICT HAS CREATED FOR CONCUSSIONS AFTER January 1, 2012 (District 51, Colorado) -- Off to a Good Start
History of Jake Snakenberg and the events from 2004 to now:
The Denver Post's Ryan Casey reported beautifully on how Jake's school psychologist, Dr Karen McAvoy's life changed with the phone call from Jake's athletic trainer about his death, and I encourage using the link at the bottom of this piece to follow and read the entire piece. "I remember greeting the freshman football team, all in tears, in the auditorium first thing on the following Monday morning. I was there as their psychologist to help with grief. It was almost unbearable."Dr. McAvoy was unaware, while she was immersed in helping others cope with this devastating tragedy, that the course of her own life would be altered as well. "Jake changed my life that day," she said, "I didn't know how extraordinary, and just how profound those changes would be."
"With a broken leg or whatever, they see the cast, they see you're on crutches, so they automatically know what's wrong," Courtney said. "But when you don't have anything to show that you're injured, people just lose sight of how serious a concussion can be, because you can't see it."
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
This forum is provided to allow members of Lumigrate to share information and ideas. Any recommendations made by forum members regarding medical treatments, medications, or procedures are not endorsed by Lumigrate or practitioners who serve as Lumigrate's medical experts.


![Expand cart block. []](/sites/all/modules/ubercart/uc_cart/images/bullet-arrow-up.gif)


Details of my personal history with brain injuries / neurological/ medical impairments and approaches to treatment and management
The reason for my concern about people whose brains have trauma being properly treated is not only because of my years as an occupational therapist, it is also due to my personal history with head/brain injury. In my twenties, before my learning disabilities were diagnosed and treated, I was 'plugged in' to try to lead a 'normal life' -- I was going to college, working, married, and in my mid 20s, had my teen-aged step-daughter move in with us one summer and the next spring my mother suddenly and unexpectedly died on a rare week when she was home without my father around. The element of having a relatively gruesome situation afterwards layered to not having any professional support as you have if someone dies with forewarning (hospice and palliative care), lead to me having a health crisis at age 29. Not only was I trying to keep all those "balls in the air" with my brain not having 'stereo vision' (I wasn't able to judge how fast a ball or car was coming towards me, or how far something was away, just as a person with sight in only one eye would have), my husband had severe seizure disorder, at least partly as a result, most likely, of an injury from junior high physical education class incident. But in the 1980's, and in your 20s, you don't think about what too much stress can do to a person.
My life dealing with a brain injury was from 'day 1' and a 'difficult birth' which was rectified with forceps since I was born in Denver in 1960; sadly this was due to the obstetrician's scheduled 3:00 pm tee-time for golf on a beautiful spring Saturday. Ironically, my parents had wished for good weather and a weekend since my father worked in Denver for Gates Rubber Company. They lived in the mountains where an early April had, in recent years, overwhelmed even the county road-crew's equipment, and until the mid 1960s, they didn't have the money to purchase a 4WD and plow for their driveway. Fortunately, the year of the 'big April Fools Day snow', my mother's cousin had not yet passed the Colorado Legal Bar exam and was staying, with his wife and child, at the property, so they had shoveled their way out. I find it so ironic that what everyone wished for with weather and day of the week for my birth resulted in something which for me, has not been so fortunate every day since.
However, it has provided me with a unique fund of knowledge and perspective about disabilities and treatments which are actually an advantage to me and those I work "with" or "for"; not only do I have an 'insider's view' of of the technical aspects, I have true empathy and understanding of how this affects a person's life in all ways, including financial. I also have a unique perspective about 'the systems' at play and can truly say I have had to face the challenges of "do I file for disability or not", "bankruptcy as the best solution .... really.....? me? .. I never thought this would happen to me' AND the worst one "if every day ahead were like today, would I want to be here?", and trust me, when the answer to that is 'no', it's just a horrendous place to be. All that was about a decade ago, and I have managed to navigate out of all of those situations in what I can only describe as a story filled with windows and doors opening and closing which lead me down a hallway and through a school of learning which now serves me well for uniquely guiding others.
In my case, related to brain injury and learning/performing cognitively or physically in school, I compensated well enough, and graduated high school with only the concern of my 2nd grade teacher, who had singled me and two others out for complicated, high-tech testing at the administration building in 'town', but they didn't have an expert to interpret the tests contracted at the time, and I "slipped through the cracks". I started to figure things out at age 29 when finally diagnosed with many visual-perceptual problems that responded well to vision therapy; I was finally fluid enough financially and aware of the expert I needed to go to. I'd actually been living for a few years with putting the suggested amounts of money into savings each month, and always had the remainder of my "college fund" banked. This has lead me to recognize how our health is truly a factor of not just having the financial resources, but the value we place on how we spend our resources, which can be insurance benefits and money.
Time and energy also factor into the equation; you always look at resources with people as time, energy, money/financial. But the person becoming aware of the products and services/experts available to them and appreciating their need for that type of service and what it can do for them completes the story. In 2007 I saw the need to start a website that would house the product and service experts who I refer people or organizations to when working with them.
Again, I find it helpful to use my case as an example: I'd known since the time I started struggling in school in sixth grade about the type of optometric specialist that ended up being a key to my being able to have further success as an adult, but since 'the experts' -- parents, school personnel, medical providers -- didn't usher me in that direction, I didn't know it was THE missing key ingredient in my life! Fortunately, when my health 'collapsed' at age 29 from being in chronic wellness into chronic illness, in the form of what is called today "chronic fatigue syndrome", my eye muscles were affected by weakness as well and couldn't compensate as they had when I was closer to chronic wellness. So I went to the yellow pages of the phone book and saw one advertisement in my small city for an optometrist who offered 'vision therapy'. The seed that was planted in my childhood about specialists NOW 'registered' with me as where I needed to spend my time, energy and financial (money and insurance) resources.
I was 29, and had reached a point in my mid 20s when I had a full time job and husband with a full time job, where I could put the recommended amount of dollars into savings. A few months of hard work and appointments, different types of eyeglasses than I'd had before (a bifocal), and additional education about my strengths and weaknesses with various types of information allowed me to have academic success finally, and I was admitted to the occupational therapy program for the 1996 graduating class.
While studying about pediatrics in the program, the "layers of the onion" continued to peel away for me when we studied sensory integration dysfunction. "This sounds like me!", I thought and sure enough, our internationally acclaimed specialist teaching the subject got her hands on me for 1 minute and pulled me aside and let me know what her observations were of my brain/body neurological dysfunction. Those home movies of me as a child where people used to remark how 'cute' and 'sweet' I had been, now were helping me to see a clearer picture about what might have happened. Once I learned what 'shaken baby syndrome' looks like, more pieces of the puzzle started to fall into place. And it's continued to be a process of unfolding what is causing what, and what can be done about it, then making decisions about how to best spend time, energy, and financial resources to correct it, while still 'living a relatively normal life'. It's helped me refine my approach to consulting related to how people occupy their time ("occupational therapist") to utilize the mind, body, spirit approach of integrative medicine.
Hence, I've paid attention to statistics about Cesarian births over the years and found the reduced learning disabilities that result interesting. I've more recently studied the obvious SMILES of people and what that tells us about their cranium/head developing, which has to do with many things but mostly nutrition. Ironically, the most obvious things about people all around Earth are, in the United States, not appreciated as diagnostic tools for what is going on inside the body. At the age of 50, I finally pursued a consultation and treatment with an expert on something I'd known about for a few years -- TMJ, but I didn't perceive my dysfunction with my joints of my head as warranting help! However, when I saw the expert present about head-forward posture in children being related to breathing problems, that rang a bell for me and I'm happy to say, I believe I've gotten to the core of the hormone tissues and system aspect of my brain/head-related difficulties.
Other issues 'at birth' have also been lessons learned for me through my personal life before I was an occupational therapist: My previous husband had been born and treated at the time as "Rh negative" and went on to be a very healthy youngster and a particularly talented hockey star in Minneapolis/St Paul; the Minnesota Star had called him 'the next Gordie Howe' when he was in junior high. He was hospitalized in that timeframe after a 'severe concussion' obtained not in his high-level hockey in or out of school, but in PE class, where he was paired with a less agile, and much larger, boy to be the "wheelbarrow" in a race. The teacher had thought it would be a way of averaging them out so that the competition would be more fair, I was told years later.
Physics is physics, and he was basically rammed into the gymnasium floor, causing a severe concussion resulting in hospitalization in a dark room for days being monitored. By late high school he developed seizure disorder and hydrocephalus which greatly impacted his life from that point on. Was it one, the other, the combination of those two significant factors plus all the other smaller ones nobody ever 'identifies and remembers'? The later, in my opinion. For two years at the end of my time wrestling in the insurance-based medicine system for occupational therapy, I employed/teamed with an incredibly gifted OT assistance who had specialized in California with a hand therapy clinic. We had many occupational health/workers compensation cases/patients and, while their jobs would require them to work differently to rest their injuries to joints or tissues while they would heal, their use of their hands outside of work for their personal lives of activities of daily living were also contributing to the problem. This included avocational hobbies. Our system has some built-in problems as it exists today, with the multiple funding sources for the different aspects; ironically a 'kitchen lady' is going to not be returning to full duty until the next school year because at home they don't have a team around them to do the heavier duty tasks! And overall, there were many things that would have helped everyone's joints and tissues from complementary/alternative medicine, but that isn't what insurance-based medicine directs people to. So I created Lumigrate to provide much of that information for people to benefit from related to these types of issues.
These things in my personal life have given me a unique perspective about many aspects of medical impairments, their treatments, and the possible outcomes. While I was studying occupational therapy at Colorado State University, I took advantage of a 50% discount for a 40-hour course to become certified in the Assessment of Motor and Process Skills, or AMPS. By the end of the course, you've become skilled at assessing human function through videos and getting a 'standardized' idea of "what is what". I might watch someone drive and say 'that is really dangerous, they should not be driving' and another OT might say 'that was not good but they cannot eat if they cannot get to the store'. While driving was not one of the tasks used to assess people, the tasks we would view and then 'rate' would be analyzed according to the standards and then we'd have a 'severity rating' which in the future would be factored in whenever we assessed someone doing a task. In actuality, it was too cumbersome to use in insurance-based occupational therapy after Medicare went to the prospective payment system (which I'll simply call 'fast-paced'), but the concepts are universally useful. And most of all, I had the exact same severity rating as the PhD who developed the AMPS! That was the first indicator I had about what would end up being my 'professional forte', of analyzing situations and providing feedback of solution possibilities and recommendations in a variety of ways.
Within a year after graduation, in my first job working for the nation's largest therapy contractor at the time, Novacare, I was being utilized by a Denver area 'retirement community' they contracted with to advise their administrators related to which level of assistance their customer's would do best with. Staff and resident trainings on various aspects of function and adaptation/compensation followed, and when the Centers for Medicaid and Medicare announced their future cost-saving program called "PPS", I foresaw the layoffs which came -- 50% of therapists were not employed as therapists in the late 1990s, many people do not know this because it was not covered in the media.
As soon as my hours of work dropped below 40/week, I started looking at how to get into another facet of employment using my OT degree and skills combined with my decade of program administration at Colorado State University and was fortunate to be in the right place at the right time to find a small, innovative driving program which was working with increasing numbers of special needs clients, young and old. The process was simple yet complex: Meet with the person 1:1 to get their history and explain our program's history and philosophy related to the brain/body as it applied to the challenging task of driving an automobile, and then provide a plan of things that could be addressed. That might mean getting an easier vehicle to drive and going to the doctor or other medical professionals for more, less, or different treatments, but it always entailed doing activities/exercises which increased the brain/body connectivity. Then in most cases that proved useful and we'd then go to the pavement and a special car then to their vehicle to further integrate and build the brain/body responses. In most cases, the person was able to successfully complete an on-street program or at least a one-time evaluation and demonstrate proficiency. This was the opposite of what we all know happens at DMV; the company was started by a man whose daughter had been killed as a passenger in a situation where two ineffective drivers collided. The standards were quite high.
The 'end of the road' for having a driver's license, is generally the most feared part of aging for people. The American Medical Association (AMA) and the National Highway Traffic Safety Administration (NHTSA) had been on the ball and collaborated in the 1990s to create an awareness and mandate about medical doctors' responsibilities about driving privileges. While this is good overall, it created some difficulties. For one thing, it's a very complex task to assess, hence the need for specialists such as myself and those I confer and collaborate with who are Certified Driving Rehabilitation Specialists. So there are solutions for that complexity -- refer them to occupational therapists who understand driving as a specialty!
The bigger problem with doctors having this responsibility is also served by their referring out related to driving: the physician/patient relationship needs to be a place where the patient can honestly tell their provider what is going on with them in order to get treatment, and if they are concerned they're going to lose their driving privileges by letting their provider know of their medical impairment and how it's affecting their function, the health and well-being of the patient is not served ideally. Again, my personal history brought this to me because my father, who died in 2010 of a progressive neurological disease I was first aware of in 1996, would not seek medical attention until he could no longer drive or live at the assisted living level as he had since 2000. When I asked him after he was properly diagnosed and treated, with good result, yet too late to really do much long-term, he stated the fear of losing his driving privileges. Again, I learned a great deal from this personal situation, and most of all learned how much more difficult it is to operate as a family member on a medical team for a patient, in particular the 'lowest one on the totem pole'. VERY different than being the primary/lead occupational therapist or a consultant from a professional aspect.
Many medical impairments, which people often mistake for going hand in hand with being older in years of life, do lead to the unfortunate reality of a person needing to surrender their driving privileges. This is best done with them involved in the process and volunteering to do so; unfortunately, often times the impairments they have make them incapable of coming to the conclusion on their own and the family, a physician and the government needs to collaborate in order to do it. While it is the epitome of 'difficult', having a specialist they go to who becomes the 'bad cop' essentially, was very helpful. I consult with people on a variety of functional topics and want people to come back and use my services again when they need to, so even I work collaboratively with someone who specializes in driving rehabilitation and has bigger credentials and much more experience than mine in this area. Not only are we getting a bigger pool of knowledge, I remain the 'good cop', or at least the cop in the middle of the intersection. If you look at the Lumigrate You Model, I'm effectively working as the surrogate to YOU, or in other cases, 'collaboratively' as You. I basically am an extension of YOU. You might look at it as your asking the question "If I had all the life and professional experience and training I have had, what would I be doing?" Or for other professionals and business or organizations who have customers/clients, I provide input. Disability cases are another facet, sometimes those have to do with brain injury and other times it's overall function from other medical impairments.
When it comes to companies with a small or large number of residents somewhere on the continuum of being safest living at the 'independent apartment', 'assisted living', or 'skilled nursing' level, having me providing an 'outside opinion' proves helpful to the organization's relationships with their residents and extended "framilies" as well. It is someone indirectly associated with their organization helping them make the recommendations and decisions. Today, with the diverging and changing economic realities in the United States, there often are different solutions which are most beneficial or necessary: increasing numbers of people are being cared for in the home by families and friends ("framily"). I went to a blues festival in Telluride and a whole group of middle aged people were wearing creatively done and humorous T-shirts about getting older and an assisted living which I'd never heard of. They were all childless professionals who were concerned about when they grew older and so they had pooled their resources and bought land and were going to create their own collaborative home to care for them, and then others, when they needed it in the future! I personally had looked at the restrictions in the US for elder care and thought 'your money goes a lot further in foreign countries', but I'd never thought of creating a communal home with your friends in middle age to prepare for old age. So, today, there are many more avenues for people when embracing end of life or medical impairment, which is an interesting challenge for me sometimes. In 2010/11/12 a person I'd been asked to consult about went from living in an assisted living to being court ordered for legal and medical guidance which was successful with getting the person living independently and at least for now, without the need for court-ordered professional management, although I will not be surprised if I get another call in the future asking me to hop back in again.
Lumigrate's initial content and foundation of information addressed a condition I have dealt with most of my adult life, chronic fatigue syndrome and fibromyalgia (CFS/FM). After having a severe case of CFS whallop me at age 29, partly from not setting good enough boundaries about my time/energy heading the administration for a researcher who was on his way, with our direct team and many others in government and the private and nonprofit sector, to the Clean Air Act Amendments of 1990, I've been able to continue working in modified ways. I'd found strategies and treatments which allowed me to return to college and become an occupational therapist and have the career I have. This was a combination of taking advantage of having good insurance and primary care through 'conventional' medicine, and 'alternatives' which were 'complementary', sometimes referred to as CAM, or complementary and alternative medicine.
Through 'functional medicine', finding the underlying cause for something and addressing it through an "integrative team approach' where collaboration is the cornerstone, people can have a return towards chronic wellness from illness with very complex issues which baffle the typical medical provider operating on their own. So I saw in this upcoming rollout of the new Law many similarities of problems and solutions.
Many people who have CFS/FM have also had head injuries in their past and part of the illness includes an awry hormone system which comes from the pituitary/adrenal/hypothalamus "axis". That's a whole topic until itself, but there is some overlap related to this topic of 'brain injury', and certainly one of the things I would like to see prevented in people who have had head injuries is their going under-treated or un-treated and developing CFS/FM. Same as with the dementias, and perhaps our recognized medical system is starting to piece the common threads together of these conditions and allow us to more effectively treat or, ideally, prevent the underlying reasons.
There is a dramatic increase in numbers of young people being diagnosed with CFS/FM and more middle aged people with early-onset cognitive impairment and even "dementia". Overall, what I've learned with the various 'cases', which I like to call 'people' I have worked with over the years, if you get them to tell their story and guide the discussion, you'll be able to unravel the mystery. Almost always you can get the yarn rolled back up into a ball, and usually you can go about creating a new 'fabric'. Please take a moment to look at the Lumigrate logo; integrating / weaving ribbons represents that aspect of my work.
As this topic was specifically about brain injury, the younger women and men I have worked with who have chronic fatigue and fibromyalgia had symptoms in their younger years and often were highly athletic and in sports which would tend to have a lot of jarring and concussing to the head. The young women often had symptoms of hormone imbalance far back into their teens and younger sometimes; again, something I relate to from my personal history. I couldn't sleep as a child, I was extremely skinny despite eating everything I could get my hands on at meal-times. Even as a baby, I would grab everything being passed around the table at dinnertime, I was later teased, not just told! In the 1960s and 1970s, not much was known. Today much is known, it's just not always known by those the public turns to or is provided to turn to for guidance. Lumigrate is here as my biggest tool to offer to my clients and others who are inclined to utilize it as well, and I'm here to help people or their teams and organizations solve more complex functional questions and situations.
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
"Occupational Therapy", a brief overview and trends leading to resurrection?
Most people don't know what 'occupational therapy' is and often they have heard the antiquated definition of 'above the waist' that's been 'out' for as long as I've been an OT, which was 1996/7. Anything that occupies time is an occupation. Somewhere in the past, people started calling how you make your living your 'occupation', which is incorrect, that is 'vocation'. Think of all the forms you've filled out that ask for "occupation" when they meant "vocation": it's caused a lot of misunderstandings and contributed to a lack of appreciation of the profession, in my opinion.
Occupational therapists work with babies nursing after birth if there is a difficulty/problem: eating is an occupation. They work with people at the end of life in palliative care and hospice, as people still have their time being occupied needing to do things for self care and leisure/enjoyment. Being able to work a remote control for the television or using the telephone are 'occupations'. Whenever there's a difficulty, occupational therapists' speciality is to find strategies or tools to increase functional independence and outcomes. I wish our profession had rebranded themselves long ago as 'functional' therapists and I have titled the OT Forum on Lumigrate "Occupational/Functional Therapy" as a result.
It is my suggestion that occupational therapists be considered to help fill these roles, as well as other qualified professional 'types'. OT as an entire discipline appears to have been omitted from this entire movement, at least i it's preparation phase. Am I surprised? Nope! From the time I learned of OT in the early 80s to the time I finally went back to get a degree in it, it was appauling to me what changes occurrred. Being new to the field, it took a while to figure out what all had gone on and what was continuing to go on to cause the changes. Talking with experienced elders in the field once I got to Colorado Springs for work was helpful; two of them write with me in the functional/occupational therapy forum.
I've attended an hour-log CME training about it and spent about an hour or two reading online and never saw the word 'occupation'. I'd recently been following the return to the public view of Congresswoman Gabby Giffords, as she was approaching the one year mark after her brain injury from a gunshot wound in an assassination attempt in early 2011. Physical therapy was mentioned. Speech therapy. Music therapy. But no 'occupational'. And considering OTs provide solutions to challenges for what occupies a person's time (24 hours a day), it is just so very amazing how we have been pushed out of the insurance-based medicine "equation!" and
and  and
and  for my historical profession but
for my historical profession but  since I had the
since I had the  to go in a private pay consulting/advisory/education capacity with Lumigrate.com as a platform for education working with PEOPLE, which is why I went into this field in the first place!
to go in a private pay consulting/advisory/education capacity with Lumigrate.com as a platform for education working with PEOPLE, which is why I went into this field in the first place!
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
Grand Junction, Colorado has gotten a lot of press in the last several years or so, for having created a system in our community through several organizations and the way they interact and collaborate, leading to better outcomes and lower costs which translates into healthier people and budgets.
I moved all the way west to Grand Junction in 2004, the same year Jake Snakenberg later died of SIS. "Junction" is located about 24 miles from the Utah border, and I had spent my entire life on the Front Range of Colorado. My 'formative years' were spent in the mountain town where the creator of South Park followed in my 'seats and lockers' ten years later and I spent 18 years in Fort Collins where I attended and/or worked for Colorado State University working in key support staff roles in statistics, air quality research and health education and studying business and occupational therapy. Graduating in 1996 from the top-rated OT program at Colorado State during the years it was so competitive only 1 in 6 applicants was admitted, I re-entered the work force this time in medicine with confidence from my previous years, mostly known for my abilities as a liaison between researchers and administrators for a now-famous research program. I was the 'right hand' to a well known and known to be difficult researcher, who I am pleased to say I'm friend with to this day. And not to worry, he likes the reputation and will be flattered I include him here to underscore how the medical system compares!
My head SPUN when I got into the Medicare/Insurance-based medical world! One of the liaisons for an industry/government consortium which collaborated effectively to move air quality forward in the past marveled after being at a meeting with my former boss at how I'd been able to work there so long! He was a get-it-done on minimal staff kind of guy, and I was continuing to grow professionally and appreciated he'd seen the ability in me at age 24 when I applied without a college degree when his my predecessor was going on to become one of the VPs of CSU. I literally had to seek out a top specialist in the US related to further treatment for visual learning disabilities and through that I found out I had a head injury, at the age of 37 after struggling increasingly starting in 6th grade and really hitting a 'wall' in college at the age of 18 and I had many difficult years after that before I got things figured out and back on track and returned to finally be 'successful' in college. I'm proud to say that US expert is one of the providers on Lumigrate's forums, which is available to help related to head injury remediation education!
However, within a year of being an OT when PPS was rolled out by Medicare and put many of us out of work and out of business providing therapy services, I actively looked to get back into administration but my 'health care' degree disqualified me in the very competitive job market. So I took the job I referred to above working in the specialty area of driving, which I am now GRATEful for due to the experience I got with teens and head injuries at a very 'high level' of functioning related to returning to driving or beginning to drive.
This turbulence lead me to have a lot of "enriching experiences" for the first 7 years of my OT career by pushing me through a variety of health care environments and teams in faster fashion than I would choose to go: I'm "of the old school" of staying at least two years in every job if possible, which is no longer the way the world works and certainly not the medical world. I now appreciate this having happened as I gained a LOT more experience, but naturally it was very stressful. Many of the jobs entailed a lot of driving/sitting and my health suffered as a result.
This leads today to why I have so much concern about how this new law and process is played out and affects people, and why I am writing this piece and launching a whole facet through Lumigrate about head injury as a result. When the providers don't have time the patient suffers the consequences; I believe this from my experiences both professionally and personally in the medical system. I have experienced first hand, the costs directly and indirectly in having things which are treatable go untreated early on. An ounce of prevention IS worth a pound of cure in this situation!
I formed my own company within a year of moving to Grand Junction in order to provide contract occupational therapy services to the therapy clinic in one of the entities responsible for getting Grand Junction on the above-discussed 'health care map' in the United States. The behavioral health practice in the building/organization was co-owned by Dr Chris Young, who also had military medical experience, as did I from doing the final internships in physical and psychiatric medicine at the Denver VA. Naturally, with the wars going on there was increased awareness about veterans returning with head injuries and that will continue in the future, as we all hopefully will be respectful and raise our awareness of how the head injuries can affect people's actions and lives. Between the increased information in the media about head injury in veterans and the new focus on youth in schools, this is a GRATE time for much improvement for our future health and related finances in the United States.
Dr Young, who is part of the consortium here in the western slope area related to best implementing The Jake Snakenberg Law, had collaborated with me founding and leading an educational group related to fibromyalgia and chronic pain/fatigue and in a very short timeframe, we had a successful group of patients/consumers who came to learn and all the providers they were interested in hearing speak agreed to come. However, with the exception of Dr Young, none of providers came to be part of the process unless they were the featured speaker and then due to an unexpected retirement of another male therapist, Dr Young could no longer afford the late afternoon hour time which was a good time for people with CFS/FM. So I got the idea for Lumigrate based out of that frustration as well as needing to have a way of communicating easily with people related to when meetings would occur or be cancelled. I created Lumigrate over a year's time in 2008-9, with Lumigrate launching in March of 2009 just before my 49th birthday.
What I envisioned and what has worked, is the public -- motivated about it being THEIR HEALTH and having more time to look into things than the average medical provider anymore (unfortunately) being the ones who find Lumigrate and digest what information they can from it and then printing/emailing or otherwise heralding their providers and asking for their collaboration in integrating the information into their treatments. Around the age of 40 when my health was at it's worst, my D.O.s and MDs in Colorado Springs were clearly wanting to help, one even saying 'wow, I took some time off to have a baby and now I'm so unfamiliar with how to refer related to insurances, I need to look into how to do your referral' and a month later I got the cardiac test she'd wanted to see results from. Another provider said 'oh, another patient with fibromyalgia brought me in something that I've made copies of". It turns out that wasn't really an established, validated protocol and it sent me on a goose chase.
With Lumigrate, I work to find valid information and providers, present progressive information such as functional and integrative medicine, (WebMD and many others do a good job for allopathic medicine's content), thereby streamlining the process for the public and providers who use it as a resource. AND we thrown in some FUN things along the way because I'm an old fan of Mary Poppins and 'a spoonfull of sugar makes the medicine go down', so to speak! And as 'luck' would have it, and in an almost unbelievable twist, there was an unexpected check from a generous family member, a cousin of my father who had never married and had children and had a good career bringing Title IX forward through collaboration and good leadership decades ago, had included me along with 10 or so people or programs to share in her estate. I found the check at the post office box after having left a seminar that I'd recorded with a borrowed camera and though "I wish I had the money to start a website because there's a real need and I think I can see how it would work." So things seem to have all come together for this purpose, among others.
Lumigrate's existing providers in the forums, which have amassed almost 2,000 new topics/supportive comments for discussion and education have been extremely effective helping our adult customers to better understand complex conditions such as chronic fatigue and fibromyalgia and would be able to offer expert advise to people who have head injury that might be different than the conventionally held believed 'time is the only healer of the brain' philosophy. It's an organic process where new providers become included when there's a need and we find the right person. We've grown from the five Junction-based providers you see on video, who are no longer active or minimally so, to over three dozen from coast to coast, including about ten from the Grand Junction area in a 2011-founded group known as the LumiGRATE Groove of the Grand Valley. (Find it in Forums on Lumigrate or on Facebook!)
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
Applying "The Assessment of Motor and Process Skills", a Tool for Occupational Therapy Evaluation and Treatment, to Young Athletes
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!