There are no products in your shopping cart.
PTSD - Post-Traumatic Stress Disorder and YOU!
How much does PTSD affect YOU? Like anything, it affects our entire society, directly or indirectly. Most people today are aware of PTSD, and some have gone beyond awareness to have knowledge about it, beyond that it stands for Post-Traumatic Stress Disorder. Still, I have people sometimes say "what's that?".
Increasingly, people becoming more educated are the ones 'diagnosing themselves', which is a first step to being able to solve a problem, as defining the problem and being able to research on key terms is 'the name of the game' today. If QUALIFIED professionals are available for the consumer/patient/YOU! to put on the team to help verify and guide treatment and education, all the better. However, today, increasing numbers of people have no professionals available to work with due to lack of expertise in their communities, lack of insurance and funding, etc.
I wanted to provide a topic and set up links to information we have at Lumigrate, as well as bring more information here to guide those who are seeking information here. In my formal training and career as an occupational therapist, I was fortunate to get quite a lot of experience with professionals who specialized in working with patients with PTSD. My internships at the Veterans Administration included 12 weeks working within the psychiatric unit, where the OTs ran a group that met three times a week, 52 weeks of the year, for veterans with PTSD. It was one of the most meaningful educational experiences of my life so far.
Another significant chapter came from the two years I worked for a visionary, progressive and solid private driving program/'school', as their founding director of rehabilitative driving services. I am setting up the link here for your information: The founder of the company gives a very nice performance in his video and the website is a wealth of information and fun to learn from: in the past, there was more emphasis in the company placed upon helping people who had been in crashes and had 'phobia' about driving. Mr Langford was a teacher to me of what amazing things can be done for people when insurance is not dictating what treatments are provided; I became certified in two 'levels' of Brain Gym™, and it was from him that I first learned to utilize The Lemon Exercise you'll see provided in links, below, via Dr Paula King, our Guided Imagery and mind/body psychology expert at Lumigrate. www.masterdrive.com/
We would set our clients up on their first visit, if they had anything interfering with their present due to their past experiences, to learn to not only do mindfulness meditation and get into a relaxed state of mind, but then to utilize imagery of the situation that had occurred, bringing in as much detail from the senses at the time --- smells, sights, sounds, skin temperature, etc. -- and then instead of the traumatic event actually occurring, visualizing something happening which diverts the situation. The intention is not at all to 'forget' what actually happened, but the brain/body essentially is reprogrammed. An example was a woman who had been hit and injured by a car of a certain color. In her visualizations she practiced, over and over again and reprogrammed her response to seeing that color car coming toward her, by visualizing that once the car got near to her, it not only didn't hit her, it had a clown in it that made her laugh. This was the experience I got from 1998 to late in the year 2000.
Back in 1996 at the VA's "psyche unit", I also would be on the collaborative care team related to any patients that were getting OT services, so I'd get to be part of the discussions with the psychiatrists, psychologists, social workers, etc. I wasn't educated about what medical model they VA used, but it was the foundation for my operating in a more 'collaborative care model' way in my career after graduation. Fortunately, about a decade later I was to connect with the brain/pain psychologist in the building I contracted OT services to in Grand Junction, Colorado, where the You! Model was to be created that you see today as our cornerstone at Lumigrate. 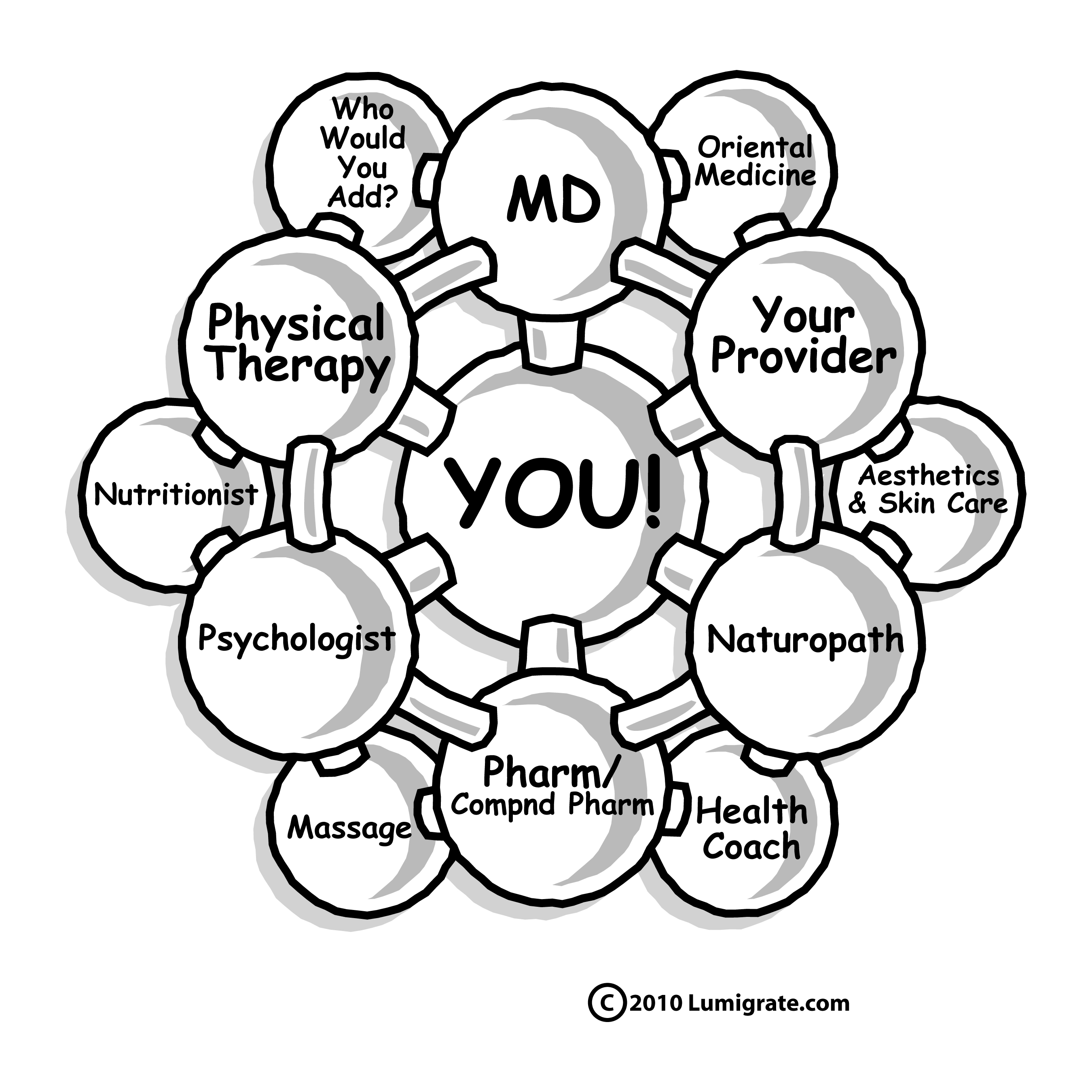
Years later, I would have a significant relationship with a Vietnam veteran who was diagnosed with both PTSD and Agent Orange exposure (toxins) and not only apply what I learned years before at the VA, but continue my education 'in the trenches of life', which truly is always the best way to get REALLY familiar with any type of condition. In his case, life had been filled with stress and trauma in his formative years, and he spent his 21st birthday on guard duty, with his C.O., who he was not fond of, bringing him a much-appreciated hot cup of coffee and saying 'Happy Birthday'.
Working to become a good husband and father and 'provider', including getting a college degree in middle life, the pressures of life combined with marijuana not being legal for recreational or medical use, meaning it would affect his employment which affected his retirement, became one of the key issues in his life during the time we spent time together on the path of life. It is because of that experience that I have the opinions I have about that particular drug, which in my state of Colorado is newly legalized and to be regulated and treated similarly to alcohol. It will be, I am sure, an interesting transition which will affect other states and the overall country (USA).
Suffice it to say I also came to see the drug alcohol, which had been part of my life since before birth, as my mother drank while pregnant, in a different light as well. And in all of this, now that I have studied more about wheat and gluten, I believe ALL people I am referring to here were incredibly impacted by the effects of diet, in particular wheat and gluten, as components after digestion get through the blood-brain barrier and influence much within the brain. It turns out, there were studies done in the VA and with the NIH (National Institutes of Health) as far back as the 1960s that indicated that gluten had a profound role in mental illness, when studied on people with the schizophrenias.
Yet, despite incredible results (50% less time to discharge from the psychiatric hospital, with evidence of one patient being totally cured) the findings from those early studies was never utilized to form bigger studies and perhaps intervene when I was a child, related to our diet. Think about it -- fifty years ago almost, this whole diet-related problem with health being impacted with literally every chronic illness, could have been resolved. In the years after, "The Food Pyramid" was put forth by the US government experts and advisors, which had recommendatings for eating grains which, on the other hand, had been shown to affect health negatively, including mental health.
After that time period, the wheat we eat commonly was changed to be even more impactful to the body, including the brain. So I want to present early on in this topic about PTSD my suspicions that diet not only at the time of the trauma but in the years before, including childhood, as well as the events of childhood and many other factors are very much 'integrated' with why a person develops PTSD. Therefore, taking a functional medicine approach to look for 'the reasons why' something occurs, and what to do about it, also has to embrace the whole of body, mind, spirit aspects. This is divergent thinking, that many things cause many other things, rather than one thing causes another, which is convergent thinking.
Generally, a factor that must be considered when talking about anyone having PTSD, but particularly when they have been in the military, is toxins. Why do I say 'particularly' for military? Because 100% of them have had things that not 100% of civilians have for exposure to things known or suspected of challenging the body/brain system: vaccinations are one very big condiseration.
Those with "depression", "anxiety" and other symptoms or diagnostic terms, including PTSD, are so high right now, there are more military personnel on active duty or discharged from the recent wars dying by suicide than dying when serving in their jobs in the military. I thank all who serve and served, and all who support them, and I am so very saddenedy by this information. I suggest we take the opportunity to really 'peel the onion' and look for the underlying reasons why and apply it to ALL PEOPLE, as the military experience for those from the US is truly a 'magnified' version of civilian life.
Fix Your Broken Brain by Healing Your Body First (the gut is the key); Studying two best-selling books: The UltraMind Solution and Wheat Belly. www.lumigrate.com/forum/fix-your-broken-brain-healing-your-body-first-gut-key-ultra-mind-solution-mark-hyman-md
Resources about convergent and divergent thinking is presented at Lumigrate within this topic about vaccines, as it is such a 'many variables and different outcomes for different people' and 'hotly' debated increasingly related to citizens "rights": www.lumigrate.com/forum/vaccinations-overall-where-do-you-stand-american-or-otherwise.
I also can look back and see how the 'trickle down effect' happens for framilies of those affected by any type of medical condition. I realize people reading this might have PTSD and they might be a loved one of someone with the condition.
It was helpful for me to have learned at the VA that research showed a correlation of what a person experienced in childhood determining the likelihood of their developing PTSD when in a situation that was identical or similar to their comrades. This is key when I look at what information to focus on at Lumigrate related to PTSD.
A decade before, I had been in a relationship with someone who had endured horrendous medical complications for about twenty years, with poorly controlled seizure disorder. He had developed a phobia of needles; hysterically, he passed out on our way out of his hysterectomy, the doctor thankfully catching his head and shoulders and lowering him to the ground, as he'd hit the doors that open out into the waiting room while I was tending to the paperwork and checkout. Looking up at the 'audience' of patients waiting to be seen by the many other doctors, including his, I said "Don't worry, it wasn't the medical procedure but the bill that got him!" He rose with the assistance of both of us and basically had a standing ovation.
Yes, when you go through enough medical 'stuff' you hopefully have some compensatory strategies and I learned from him about having a sense of humor about things. I never saw him be angry at his problems, perhaps because they didn't really know what caused him to have hydrocephalus. It took four years to get a diagnosis, only occurring when CT scans were available to the public in the mid 1970s, so perhaps it was simply a relief that modern medicine could address the issues, prolong life, increase quality of life.
He also had Ozzie and Harriett as parents; his family of origin was literally the 'ideal American post World War II/Baby Boom family'. His father had served in the US Army, and was in the Battle of the Bulge. Apparently he too, had developed good coping strategies as a young man, despite only having an 8th grade education, for dealing with what he experienced in the military. Yes, this is merely a subjective 'story' that I have observed in my life, but I include it to inspire others to look at the people they've known in their lives, and see what kinds of things you can take away that serves to support you in forming your opinions and then taking action going forward related to psychological trauma for YOU or someone you are assisting in life.
My father had chronic pain and chronic fatigue my entire life, and yet was never diagnosed or treated for 'fibromyalgia', only some of the symptoms. Would he have gotten a diagnosis of Gulf War Syndrome and PTSD had he served in different military times? I believe so.
My point in mentioning all this is that people are oftentimes NOT aware the symptoms they have would indicate they could be diagnosed with medical conditions, and PTSD is one of them. I interact with people all the time who, I think, would have a strong possibility of being 'diagnosed with PTSD' if they were to seek out a professional. So I will suggest people reading this, whether it's about YOU directly or indirectly, go beyond 'awareness' and become 'knowledgeable' about what PTSD is.
I refer you to this page at a wonderful website, Peace Candles, where you will find the definition from the Merck Manual of PTSD, substantiation of what I have presented related to diet, and the writer's opinions and more facts about the common treatment for PTSD related to pharmaceuticals, with a very well-written disclaimer which serves to remind us to go beyond awaress to education and forming opinions and becoming ACTIVE about what we believe to be right for us and our health, related to PTSD and otherwise.You will see there, the core of information states:
PTSD definedPosttraumatic Stress Disorder (PTSD) is defined clinically in the Merck Manual (the world’s most widely used medical reference) as an anxiety disorder caused by the exposure to an overwhelming traumatic event, in which the person later repeatedly reexperiences the event. These experiences are considered to threaten death or serious injury that can affect people long after the actual occurrence has been experienced; an intense fear, helplessness, or horror that can haunt a person’s beliefs, thoughts and behaviors negatively. Traumatic events may involve having been threatened with death or serious injury or witnessing violence against another person. Clinical examples include engaging in military combat, experiencing or witnessing sexual or physical assault, or being affected by a disaster, either natural or man-made. A delayed onset of PTSD symptoms may take months, years, and even decades to appear. A diagnosis of concurrent symptoms for 3 months consecutively is considered as a chronic affliction with PTSD. This manual also concludes that this disorder affects at least 8% of the people at sometime during their life with the symptoms of reexperiencing repeatedly, usually in nightmares or flashbacks. (1)
In lieu of .... events (since 9/11/2001), I would venture to say those percentages have risen considerably.
The Merck manual continues its definition of symptoms to PTSD, as an intense distress that often occurs when the person is ‘triggered’ or exposed to an event, situation, even conversation. Even with persistently avoiding things and people that may remind us of the trauma. We will attempt to avoid thoughts, feelings/emotions, and talking about the traumatic event, also trying to avoid situations or people who serve as reminders.
Avoidance may lead to amnesia and/or a numbing or deadening of emotional responsiveness, as well as the tendency to being overly sensitized to relaxation or stimulation (difficult to fall asleep/easily startled). They go on to say that symptoms of depression are also common, as is losing interest in previously enjoyed activities. Feelings of guilt, whether “survivor’s guilt”, ‘why me’ guilt, or the guilt associated with being deserving of the trauma. (1)
www.lumigrate.com/forum/dr-paula-king-using-lemon-show-power-mind -- a FUN, short video is presented where Dr King uses visualization of a lemon to demonstrate the power of the mind. .. and ....
Treating PTSD in Non-Traditional Ways
With the rise of psychological ailments among Iraq and Afghanistan War vets, military and VA hospitals have begun to rethink how they deal with this age-old scourge of war. Here is a rundown on six new methods of handling combat-related emotional trauma.
By Janice Arenofsky
The Iraq War veteran seated in George Gafner’s office reported only minor wounds from his time in the Middle East. But emotionally, the soldier was scarred. And traditional talk therapy alone was not working to relieve the pain of seeing his comrades killed from an explosion.
For Gafner, a licensed clinical social worker at the VA Medical Center (VAMC) in Tucson, Ariz., the next step was treating his patient’s post-traumatic stress disorder (PTSD) with hypnosis.
“People are more receptive to suggestions under hypnosis,” says Gafner, director of family therapy training and author of several books on hypnosis. “When you deal with the unconscious, you can get under the radar and help the person.”
Gafner usually starts off by strengthening the soldier’s self-esteem and lessening symptoms such as survivor guilt by floating the suggestion that “you did the best you could—it’s time to move on with your life.” Gafner also provides his patients with a physical “anchor” for triggering the relaxation response, such as interlocking fingers.
“It’s not a magic bullet,” Gafner emphasizes, “but it takes the rough edges off, and the feelings become more manageable.” Gafner says hypnosis achieves a 70% success rate and is effective with 90% of men and women. But some patients hesitate to try it because of popular associations with its practice, such as the fear of “quacking like a duck.”
Unfortunately, absurd beliefs like this have slowed the military’s acceptance of non-traditional therapies, despite that alternative medicine is now part of mainstream health care.
In fact, a 1999 National Health Interview Survey revealed that 29% of U.S. adults had used some form of alternative therapy within the past year. And a recent study shows nearly 50% of veterans also do the same.
That’s one reason the Department of Defense funds the Complementary and Alternative Medicine Research for Military Operations and Healthcare Program. It has researched such treatments as manipulation, bioelectromagnetic devices and acupuncture.
Moving on With Meditation
Turned off by talk therapy and medication, some veterans have gone the alternative route. According to former Army Spec. 4 William A. Roper, a 59-year-old Vietnam vet who received a traumatic head injury, meditation helps him cope with survivor guilt and memories of war atrocities.
“I do it twice daily, in the morning and evening for 20 minutes,” Roper says. “Meditation calms your raging mind and allows peace to permeate your very being,” he says. “In time, you heal, the awful memories subside and you get back control of your life.” Roper also says a positive can-do attitude “internalizes the idea that you can overcome your situation.”
Vietnam vet Claude Anshin, author of At Hell’s Gate: A Soldier’s Journey from War to Peace (Shambhala, 2004), agrees. After PTSD turned Anshin into an alcoholic and drug abuser, he sought relief with Buddhist beliefs. Today, he spreads the word about meditation’s healing path by holding retreats for traumatized veterans.
Soon to recruit volunteers are two VA clinical studies on mindfulness meditation and directed meditation involving Iraq/Afghanistan War veterans and women veterans who have been sexually traumatized (especially in Iraq and Afghanistan).
“Mind-body approaches such as meditation are non-invasive and, unlike medications, have no risk of side effects,” says Dr. Jennifer Strauss, with VA’s Women Veterans Comprehensive Health Center in Durham, N.C. The principal investigator of the female PTSD study, Strauss says meditation is “empowering” because it’s “done by” rather than “done to” the patient. Also, self-guided therapies can attract patients who want to limit travel to and from VA clinics.
Strauss’ 12-week program emphasizes guided imagery. After an initial session with a licensed clinical social worker, the patient listens to audio recordings of imagery instructions. So far the study shows that guided meditation significantly reduces PTSD symptoms and compares favorably with the results from psychotherapy.
Music Therapy
Sherill F. Cross, registered music therapist at Waco VAMC in Texas, runs a VA music therapists network there. Although Cross works with only 100 patients each year, similar music-therapy-directed relaxation training is available at many VA hospitals, such as in Houston, Topeka (Kan.), Milwaukee and New York.
“They [soldiers] have just returned from a [combat] situation where they’ve been hypervigilant and had screwed up sleeping patterns,” Cross says. “They need help in dealing with issues and resetting their pattern to ‘default.’”
Cross begins her 10-week program with individual sessions, teaching patients to focus on breathing while listening to slow and lyric-free music. Meanwhile, she instructs them in a 20-to-30-minute relaxation exercise, such as progressive muscle relaxation, or uses guided imagery (“put yourself in a bubble,” “imagine yourself as a rag doll”).
Cross has helped several women vets by suggesting the use of simple instrumental music while taking a warm bath. The women’s sleeping, communication skills and self-esteem improved.
“Ninety to 95% of PTSD patients are clueless on how to relax,” Cross says. “They’re afraid of intrusive thoughts and memories.”
When they begin to feel emotions, “thorns” (problem areas) often emerge. When this happens, Cross suggests patients talk to their treatment coordinator or one of their peers. “I tell patients to let the music take you where you want to go,” she says. “I give them permission to stand down.”
Cross steers away from music popular during their deployment—for example, for Vietnam vets, Otis Redding’s “Dock of the Bay” and music from the films Forrest Gump or The Big Chill. “A big step toward recovery is separating from this old music,” she says.
Animal Therapists
Carol Triesch may not be a licensed psychotherapist, but her golden retriever is. Certified by Delta, a Washington-based organization that promotes the bond between animals and people, Jasmine instinctively knows how to break down vets’ emotional barriers. “Some of the soldiers [at Brooke Army Medical Center in San Antonio, Texas] are on the burn units and have open stumps that smell differently,” Triesch says. “But Jasmine doesn’t sniff at them and make them feel self-conscious.”
To the contrary, Jasmine and Triesch, who together earned the title “top therapy team in the U.S.,” seem to have a “cathartic” effect that releases pent-up stress. Soldiers often talk over their war experiences with Triesch while they pet Jasmine or teach her a trick. “Former snipers and special operatives touch Jasmine and melt,” Triesch says. “Sometimes they cry.”
The team also lightens up the hospital’s stark surroundings with outrageous outfits that transform the caring canine into a rubber duck, for example, or a Christmas tree. David Frei, a veteran, American Kennel Club judge and animal-assisted therapist, recently observed Triesch and Jasmine while he was filming them for a TV program.
“The dog was a wonderful motivator for rehab patients,” says the Westminster Kennel Club communications director. “After 21 months of rehabilitation, one brain-injured patient whose left side had been paralyzed was able to pet the dog with his left hand. Dogs can pick out the neediest person, show their total acceptance of that person and give a sense of normalcy to hospital-bound patients.”
Emotional Freedom Technique
Developed by engineer Gary Craig and piloted at the Naval Medical Center San Diego, Emotional Freedom Technique (EFT) is “acupuncture without the needles,” according to Susan Hannibal, an intuitive healer who uses this energy-based therapy in her southern California practice. Instead of using needles, therapists ask patient to tap with their fingertips at certain acupoints on their face, hands and trunk while they think of the trauma or issue. “The tapping releases blocked emotions and restores the smooth flow of energy,” Hannibal says.
A close cousin to EMDR (eye-movement desensitization and reprocessing), which the VA has approved for treatment, EFT has not yet been approved. But according to an article in the San Diego Union-Tribune, Jeannie Ertl, a senior clinical social worker at the Naval Medical Center, learned EFT from Hannibal and tried the method on 15 PTSD patients. She found it lessened or eliminated anxiety and other symptoms of stress for 12 of those patients.
Maj. Brian Stoll, a 52-year-old mobilized reservist stationed at Fort Bragg, N.C., returned from Iraq with ugly memories of mortars and ambushes. While PTSD symptoms such as anger, agitation and poor sleeping tormented him, Stoll submitted to two years of cognitive therapy rather than take medication.
A classmate told him about Hannibal’s Web site. “I prefer a holistic, non-invasive approach,” Stoll says, “but I wasn’t sold on the idea at first.”
Still, due to Stoll’s exposure to Eastern treatments such as acupressure and massage when stationed in Southeast Asia, he decided to give EFT a chance.
Last year, in a 30-minute telephone session with Hannibal, Stoll finally got relief. He was no longer disturbed by loud sounds that reminded him of artillery. “She guided my tapping, and I repeated messages of ‘acknowledgement’ and ‘release,’” he says. “I’m not totally cured, but she began to peel away layers like an onion.”
Stoll wants to continue with EFT, but the local VAMC doesn’t offer it, and he has not yet located a private practitioner.
Virtual Reality Treatment
San Diego’s Naval Medical Center funds a high-tech alternative called Virtual Reality Treatment (VRT). PTSD patients who do not respond to medication are eligible for VRT, a computer program. It was created by psychologist Dr. Albert “Skip” Rizzo, a research scientist at the Institute for Creative Technologies at the University of Southern California. Borrowing elements from the popular video game “Full Spectrum Warrior,” “Virtual Iraq” immerses patients in the sensory stimuli of war.
Patients wear virtual reality (VR) goggles attached to a helmet (the Virtual Emotion Sensor). From a raised platform that vibrates to imitate riding in a Humvee, the patient hears and feels exploding mortars, fighter planes and bullets.
Courtesy of a “smell machine” (Envirodine Scene System), the soldier also can smell different odors tied to Iraq experiences, such as garbage, weapons fire, spices, diesel fuel, burning rubber and even body odor.
“Entering VR is a stressful experience,” says Lt. Cmdr. Rob McLay, a Navy psychiatrist and director of the VRT program. “So it can be hard to get people to try it or stay with it.”
VR therapy is used to treat PTSD at Camp Pendleton in Oceanside, Calif., the Naval Medical Center San Diego and Tripler VAMC in Hawaii. At the San Diego facility, five patients completed treatment, and eight are still enrolled.
McLay says the first woman VRT patient saw her nightmares fade. “Most patients are able to recover to the point where they can go back to work and family,” he says.
Although VRT is similar to traditional exposure therapy in which the patient mentally and repeatedly relives his or her war experiences until he or she can remain calm, VRT does not depend on the patient’s abilities.
And therapists can increase or lessen the stimuli depending on the patient’s stress tolerance. Also, younger computer-savvy soldiers with PTSD do not automatically equate VRT with mental problems and stigma.
To encourage more soldiers to accept help, psychologists may classify VRT as “post-combat reintegration training.” This may be more acceptable to the 60% to 70% of soldiers with PTSD who decline treatment.
VRT sessions last approximately 90 minutes and take place once or twice a week for a total of 12 sessions. There are two types of programs—one for frontline personnel and another for support staff.
Acupuncture
Studies show that acupuncture, in which licensed health practitioners stick thin needles into certain areas of the body to release negative energy, eases stress, anxiety and pain.
It also is another tool for patients reluctant to seek help due to stigma, says Dr. (Col.) Charles C. Engel, who works at the DoD Deployment Health Clinical Center at Walter Reed Army Medical Center in Washington, D.C.
Engel, principal researcher for an ongoing clinical study on the use of acupuncture, says veterans who prefer the lower cost, absence of side effects or short-term commitment may opt for acupuncture.
According to the Samueli Institute for Information Biology in Alexandria, Va., which co-sponsors alternative medical research with the military’s Uniformed Services University of the Health Sciences (USUHS), acupuncture services are available at some veteran clinical sites, such as William Beaumont Army Medical Center at Ft. Bliss, Texas, and the Cincinnati VA Medical Center.
Dr. (Lt. Cmdr.) Susan D. Harvey says doctors at the Naval Medical Center San Diego regularly provide acupuncture for pain management, and she has treated a limited number of patients with PTSD to target symptoms such as irritability, insomnia and pain.
“I treated one combat medic with two tours in Iraq,” Harvey says. “With six sessions of acupuncture, he experienced decreased anxiety and need for pain medication and an increased sense of well-being.”
Alternative treatments can supplement traditional psychotherapy and medications. Veterans should contact their health provider to check for insurance coverage and availability. The bottom line: PTSD is a diagnosis—not a life sentence.
Janice Arenofsky is a freelance writer based in Arizona who specializes in health topics. She has written several VA-related articles for VFW.
http://www.healingthosewhoserve.org/treatment/default.asp
____________________________________________________________________________________________
Women and PTSD
Posttraumatic stress disorder, PTSD, is a complex psychological complication found in many returning war veterans. For pain management specialists, the complexity of PTSD, coupled with the management of a veteran's chronic pain, leads to tailored programs in treatment.
If you are returning home from the war and you find that you are experiencing complications associated with PTSD, in addition to chronic pain, it is important to find a pain specialist who understands both. While many vets find they return home and simply succumb to the VA benefits they are afforded, it may be necessary to move beyond this treatment and seek private healthcare from a pain management specialists who understand the implications and cyclic effect of both.
There are some within the military community who may boast that the VA is trained to treat this specialized complication of chronic pain and PTSD. However, in the civilian life, when a traumatic injury occurs, nearly 50 percent of those civilians also suffer PTSD while trying to manage chronic pain. As a result, there are pain management specialists who may be far more educated and specialized in the treatment of your condition.
Should you seek treatment within the VA system, be certain your chronic pain and psychological issues are addressed by the VA physicians. Because many returning veterans are unfamiliar with the psychological aspect of PTSD, and how it impacts their chronic pain from war injury, it may be at your insistence that testing into this diagnosis is made. Often, when managing chronic pain, the issues of PTSD are not addressed as they should, in both civilian and in VA medical care.
As with any complication that arises out of a traumatic injury, it is important to understand the mind-body connection your healing process will require. For many war veterans, the risks for PTSD are quite significant but can often be overshadowed by the chronic pain treatment administered for the physical injury. With the proper psychological evaluation, and confirmed PTSD, you can begin to heal both mind and body which, ultimately, may improve your healing process and save your marriage and family relationships.
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
This forum is provided to allow members of Lumigrate to share information and ideas. Any recommendations made by forum members regarding medical treatments, medications, or procedures are not endorsed by Lumigrate or practitioners who serve as Lumigrate's medical experts.


![Expand cart block. []](/sites/all/modules/ubercart/uc_cart/images/bullet-arrow-up.gif)


Post Traumatic Stress Disorder (PTSD) and Hypoglycemia
in Info for hypoglycemics, Related disorders on December 3rd, 2011
By Jurriaan Plesman, BA (Psych), Post Grad Dip Clin Nutr.
“An estimated 7.8 percent of Americans will experience PTSD at some point in their lives, with women (10.4%) twice as likely as men (5%) to develop PTSD. About 3.6 percent of U.S. adults aged 18 to 54 (5.2 million people) have PTSD during the course of a given year. This represents a small portion of those who have experienced at least one traumatic event; 60.7% of men and 51.2% of women reported at least one traumatic event. The traumatic events most often associated with PTSD for men are rape, combat exposure, childhood neglect, and childhood physical abuse. The most traumatic events for women are rape, sexual molestation, physical attack, being threatened with a weapon, and childhood physical abuse.
Conventional Treatment
PTSD is treated by a variety of forms of psychotherapy (talk therapy) and drug therapy. There appears to be no effective treatment, but some treatments appear to be quite promising, especially cognitive-behavioral therapy, group therapy, and exposure therapy. Exposure therapy involves having the patient repeatedly relive the frightening experience under controlled conditions to help him or her work through the trauma.
Source
To understand the development of PTSD, we need to realize that any trauma – the death or loss of a loved one, moving house, war experiences or financial crisis – will cause stress hormones to interfere with the normal production of our feel good neurotransmitters such as serotonin and others. These are environmental stresses that can result in environmental depression. Nature makes sure that we have the right neuro-chemicals to deal with the stress.
Normally, after the removal of the environmental stress people start to produce serotonin again and life resumes for most people. However, for some people this is not what is happening. They continue to be depressed for some reason not quite understood by the person. He keeps on producing excess stress hormones, such as adrenaline, that prevents him from producing serotonin. And because he fails to produce serotonin, he will also be lacking in melatonin,our sleeping hormone. Thus the clinical picture is of a person depressed and unable to sleep, waking up with sweats during the night. He may have other symptoms such as anxiety attacks and unpredictable mood swings.
It is natural for a person with PTSD to link his depression with the trauma, because this was indeed the direct cause of his depression at the time of the trauma. In fact this indelible link with the traumatic event(s) will probably amount to an obsession, as the only possible logical explanation for his physical symptoms that are internally generated by a flaw in his metabolism. It may even lead to false or exaggerated memories, sometimes amounting to delusions.
Perhaps the difference between endogenous depression and PTSD is that the latter is usually associated with a specific traumatic event. A student who becomes depressed because of exposure to stresses due to a competitive educational program is not generally seen to be a victim of PTSD, although the underlying mechanism is the same.
The fundamental question is, why is the person not producing serotonin?
If PTSD is primarily a biophysiological disorder, then we should not expect talk therapy or even Rational Cognitive Behaviour Therapy (RCBT) alone to have great success. This approach is based on the assumption that ‘psychological experiences’ resulting from a brain disorder are the CAUSES of mental illness, instead of symptoms.
PTSD may be Associated with Insulin Resistance
A possible explanation for PTSD is that like other mental illnesses, it shares a common metabolic disorder of insulin resistance (hypoglycemia), that can fully explain the psychopathology of PTSD. See References. Of course any other silent disease can be responsible for PTSD, but hypoglycemia happens to be a common one.
This can be easily tested with the special medical Glucose Tolerance Test for Hypoglycemia (GTTH). This test could also be used to predict the likelihood of a person developing PTSD prior to an expected series of traumatic events – such as a soldier going to war. If proved positive such person should be advised to adopt the hypoglycemic or diabetic diet. An alternative home paper-and-pencil test called the NBI, will also give a fair indication for hypoglycemia. Another useful test can be found at: The Hypoglycemia Questionnaire.
This also explains why some people will fall prey to PTSD whilst others don’t, because not all people suffer from hypoglycemia or other biological disorder as a precondition to mental illness and perhaps PTSD.
Hypoglycemia an Unnamed Medical Condition
Hypoglycemia admittedly is a misnomer, and may confuse traditional medical practitioners with the concept of low blood sugar levels commonly found among insulin-dependent diabetics. An other good explanation is given at: Gary Null (2002)
Some nutritional doctors have attempted to replace the term with ‘dysglycemia’ to indicate that we are dealing with unstable blood sugar levels – showing abnormal peaks and falls – rather than low blood sugar levels. The problem is that the term ‘dysglycemia’ would not explain the phenomenon of ‘cerebral diabetes’ or ‘cerebral hypoglycia’, recognized by some scientists to block glucose utilization somewhere along the biochemical pathway of glycolysis. See: Holden RJ et als 1994 and Holden RJ, 1995
Dr George Samra has called this condition “Hypoglycia” to indicate a flaw in glycolysis mostly due to an imbalance between zinc and copper levels, hence an obstruction in the production of biological energy called ATP. See here. This may occur among people with “hypoglycemic” symptoms, with normal results in a Oral Glucose Tolerance Test. (Samra,70). Neuroglycopenia is another medical candidate, but like the others wrongly assumes that low blood sugar levels is the cause. Hypoglycia is also discussed in Getting off the Hook at page 18. The closest medical term that would fit the hypoglycemic syndrome would be Syndrome X or The Metabolic Syndrome, except that the mental aspect is missing.
PTSD and Hypoglycemia
The connection between insulin resistance and PTSD can be explained because the body has problems responding properly to insulin. Insulin functions to transport glucose – as well as amino acids, and fatty acids – into cells for conversion to biological energy called ATP. The brain is entirely dependent on glucose as its only source of energy. Without proper energy levels the brain cannot manufacture the feel good neurotransmitters such as serotonin.
With resistance to insulin, blood sugar levels rise and the pancreas will respond by secreting more insulin into the blood stream, called hyperinsulinism. Increased insulin concentrations will trigger a sudden crash in blood sugar levels – a hypoglycemic dip. This is a signal to the brain (hypothalamus) that it is threatened with brain starvation. It responds by sending a hormonal message to the adrenal glands to dramatically increase adrenaline production.
Adrenaline – a major stress hormone – functions to rapidly increase blood sugar levels by converting stored sugar, glycogen, back into glucose. (See image) The reaction happens in the twinkling of an eye. The internal massive production of adrenaline – and perhaps cortisol to a lesser extent – prepares the body to face a crisis situation, except that in this case, there is no external cue to spark the biochemical reaction. Energy is diverted from digestive organs to the heart, muscles and brain, and these form the unexplainable symptoms of people suffering from hypoglycemia, anxiety attacks, phobias, depression, addictions, as well as PTSD.
The Sympathetic Nervous System is now in overdrive! With such an mysterious assault of adrenaline on the autonomic nervous system, it is no wonder that the trauma is perceived to be directly responsible for the anxiety attack. The connection between depression and insulin resistance, therefore PTSD is well documented. See here.
The Hypoglycemic Diet
The non-drug treatment for insulin resistance (hypoglycemia) is the adoption of the hypoglycemic diet, which is similar to a diabetic diet. It will normalize glucose, insulin and stress hormones and should be adjusted to the individual needs of the client, having regard to the individual nutritional biochemistry of the person. Possible allergies should be eliminated as well.
Certain nutritional supplements – such as zinc, vitamin C, fish oil, B-complex – are essential because depressed people have often been found to have specific nutritional deficiencies and requirements. Chromium picolinate will sensitize receptors for insulin and have been reported to reduce depression.
People often have the mistaken impression that hypoglycemic diet as a quick fix diet. The body needs time to readapt to normal blood sugar and insulin levels, relearn to produce enzymes and coenzymes, replenish body stores for minerals, up-regulate or down-regulate neurotransmitter receptor sites and adjust to various other hormone syntheses. Clinical experience has taught us that benefits should become apparent in about three months on this diet for most clients. If drugs have been used to treat symptoms it may take some more time for the body to repair the damage done to receptors for normal neurotransmitters.
For a full list of depression related illnesses see: Physical Causes (and Solutions) of Depression by Dr RJ Diamond. When drugs have been used, the hypoglycemic diet may speed up detoxification, especially if it is supplemented with nutrients such as B-Complex vitamins, vitamins C, E, beta carotene, B6, zinc, chromium picolinate, fish oil, and so on.
On the basis of clinical experience we have found that the effects of marijuana use on behaviour may last up to six months. (I am not aware of any studies in this regard).
When more powerful street drugs have been used, such as methamphetamine or cocaine, recovery may take much longer. One study by Volkow at als. in 2001, has suggested that receptors for dopamine can be restored between 9 and 14 months following sustained abstinence.
Pyroluria: Another mechanism involved in the development of PTSD is that a crisis/ trauma/stress may increase the synthesis of kryptopyrrole (HPL), a by-product of hemoglobin in our red blood cells. Or that the trauma may be the result of pyroluria and not the other way around.
Hemoglobin is a red protein responsible for transporting oxygen in the blood of vertebrates. It contains a iron atom bound to a heme group. Kryptopyrrole prevents the absorption of zinc and vitamin B6 as it bind with HPL and passes this out of the body in urine and causes their deficiencies. Deficiency in zinc and Vitamin B6 may cause secondary deficiencies in magnesium and manganese and raise toxic copper levels. Many of these nutrients are necessary in the synthesis of serotonin. See: Journal of Orthomolecular Medicine 1974 Some studies has failed to find a connection between pyroluria and schizophrenia[17][18][19][20][21][22] and Pyroluria Mystery explained.
Psychological Aspects
There is a principle in behaviourist psychology suggesting that whenever an animal experiences a strong emotion, without an external object, it tends to react to any object in the environment by the mechanism of REVERSE CONDITIONING. It may pick any outstanding object in its immediate environment and ‘perceive’ it as the cause of that emotion. In more technical psychological terms any neutral object in the environment may become a stimulus for the fear response in an animal conditioning experiment. The ringing of a bell may become the stimulus of a fear response if it has been paired by an electric shock in the past. A natural action by an animal may be reinforced if it is constantly paired with a command by its trainer.
In humans, an unexplainable strong emotion – such as an internally driven adrenaline upsurge – can be paired with any outstanding neutral object in his environment, and becomes to be perceived as the cause of that strong emotion. Thus we see how anxiety attacks, phobias can be created by pairing of unexplainable biochemical reactions to thoughts and to TRAUMATIC EMOTIONAL MEMORIES in the past. It is a mechanism to preserve our sanity, to provide some sort of ‘rational’ explanation.
Nutritional/Psychological treatment
Armed with this new knowledge, therapists should realize that the psychological link between an internally driven emotion and past traumatic memory helps a victim to manage his illness psychologically. He may have resorted to alcohol or drugs, or other kinds of behaviour for self-medication. If a therapist were to attempt to break the connection between ‘emotion’; and ‘past experience’ through psychotherapy or any other kind of talk therapy, the therapist would fall into the trap of confusing causes and consequences. It certainly will increase his/her client’s suffering.
In other words a therapist may unwittingly “enable” a client to believe that the “cause” of the emotional disorder is the “trauma”, whereas in fact attention should be brought to the underlying metabolic disorder operating in the here-and-now and that is generating the symptoms of PTSD.
For example, a young woman who suffers from PTSD resulting from abuse in her childhood, would be very reluctant to give up this connection, whilst she is suffering from a physical disease. The connection helps her to manage her illness and allows for a rational explanation of her behaviour for the time being.
The better psychotherapeutic strategy would be to treat the biochemical disorder first, BEFORE any attempt at psychotherapy. Thus a therapist should concentrate first on dealing with the biochemical aspect of the disease – the depression – either with the help of a doctor, or preferably a nutritional doctor or person trained in clinical nutrition. But this all depends on the therapeutic situation and should ultimately be left to the discretion of the therapist. In the case of PTSD, I feel that a therapist should wait until the biochemical imbalance has been restored, which could take quite some time. It is then when psychotherapy could be helpful in dealing with psychological problems.
The hypoglycemic diet is a powerful tool for dealing with PTSD what is, after all, a nutritional disorder. It is only when we gain some control over the biochemistry of the client that we can deal with the damage done to personality with psychotherapy.
A person who has suffered for many years with PTSD, may have developed comorbid conditions such as alcoholism, substance abuse, social anxieties and fears, lack of self-esteem or of inappropriate assertiveness, aggressiveness, and many other ‘psychological’ consequences. These can be dealt with in a course of a structured psychotherapy course.
We have a self-help psychotherapy course at this web site, but any other therapeutic approach, especially RCBT, should help clients recover from the psychological consequences of the disease, when the biological aspect has been successfully treated.
Index to Specific Topics and Research
References to Mood Disorders and Nutrition
Post Traumatic Stress Disorder (PTSD)
Depression and Insulin resistance
Depression and Genes
Diabetic gene
Hypoglycemia, Diabetes & Depression
Insomnia and Hypoglycemia and Melatonin
Serotonin and carbohydrates (sugars)
Zinc and picolinic acid, tryptophan
Post Traumatic Stress Disorder (PTSD): A Disease of Body and Mind
Psychotherapy
What is Hypoglycemia?
Nutritional Aspects of Depression
Depression is a Nutritional Disorder
Testing for Hypoglycemia
The Nutrition-Behavior Inventory (NBI)
Depression a Disease of Energy Production
References
Volkow ND, Chang L, et als. Loss of dopamine transporters in methamphetamine abusers recovers with protracted abstinence. J Neurosci. 2001 Dec 1;21(23): 9414-8. PMID: 11717374
Also: BrookhavenNational Laboraty News Release.And
Dr George Samra (2002), THE HYPOGLYCEMIC CONNECTION II, One Stop Allergies, Sydney, Australia. Page 70. Available here.
Source/link:
www.hypoglycemia.asn.au/2011/post-traumatic-stress-disorder-ptsd-and-hypoglycemia/
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
Stress Kills via Inflammation (Possibly)
I am getting more and more requests if I know any other evo med/nutritionally interested psychiatrists around. Folks are asking from Atlanta to Vienna. At the moment I know of four, including myself. Three of us are in New England and one, Ann Childers MD, in Oregon. My only advice is to keep checking Primal Docs and the Paleo Physician's Network. The three other psychiatrists I know of seem to be excellent, well-trained, and careful folks, for what it is worth. If other psychiatrists want to drop me comment (I can see it and not publish it if you ask), I'm more than happy to keep a list and to ask ahead of time if you want your name released to an interested party. We are also working on a forum for doctors to share case studies, experience, and documentation, so let me know if that would interest any physicians out there (again, can leave a public comment, or leave a comment with a note not to publish if you want to remain incognito).
Love this song (all the songs I like when I first hear them end up being advertisements for Apple. They should hire me to spot music for them, for sure…) Come Home by Chappo (right click to open in new tab).
Now, science. Overshadowed by events and personalities sometimes. I'm a psychiatrist. I'm used to that sort of thing, but it doesn't mean it is particularly fun for me. Perhaps it is less fun, as it feels more like work. But the journals march on, and it is finally spring here. Lifetime exposure to chronic psychological stress is associated with elevated inflammation in the Heart and Soul Study.
(It is so uncool to post links to Elsevier nowadays, but they have my favorite journal hostage so what can we do? Ethics only take us so far, and then we have to write a Graham Greene novel, but we are still left with what to do. This issue is the eternal crux of clinical medicine. My patient does not walk out of the files of a clinical trial, where all sorts of comorbitities are excluded, but my patient still has clinical depression and still wants some reasonable advice…)
I like the Heart and Soul Study. They are on my wavelength. The methods are solid. All the subjects have a history of some sort of cardiovascular disease, which is important (and they are mostly male, derived mostly from the VA, so keep that in mind). And here they have looked into people's history of psychologic stress, measured their inflammatory cytokines, and hypothesize a connection. The connection is confirmed by many other studies linking a history of trauma (all sorts) to elevations in cytokines.
The DL is that stress is linked to bad cytokines (IL-6, TNF alpha, C reactive protein, etc.) and that stress is linked to PTSD and Major Depressive Disorder and anxiety disorders which are also linked to the bad cytokines… as is cardiovascular disease, even in psychologically healthy individuals. In addition, there are harmful behaviors which increase the inflammatory cytokines (substance abuse, smoking), and ameliorating behaviors that decrease them (exercise, meditation, sleep) less likely to be adhered to by those who have undergone inordinate psychological stress.
Where the rubber meets the road is that higher lifetime trauma was associated with higher levels of inflammatory cytokines at baseline and 5 years later. When the researchers controlled for psychological symptoms of the trauma (for example, PTSD or a clinical depression), the relationship held, meaning those who had undergone trauma had elevations of inflammation even if their behavior and coping seemed more normal by psychiatric diagnostic standards. In these folks with pre-existing cardiovascular disease, higher inflammation is associated with greater risk of death and complication.
Maybe I should leave off and move to Hawaii after all...
Source, above, is the blog site by Emily Deans, MD; Evolutionary Psychiatry: http://evolutionarypsychiatry.blogspot.com/2012/04/stress-kills-via-inflammation-possibly.html
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!