There are no products in your shopping cart.
Lewy Body Dementia and the Association's "10 Things You Should Know about LBD" (Plus My Experiences)
Lewy Body Dementia is the generally said to be the second most common form of dementia in people in the US, with some experts will say 'second or third'. In editing this topic on March 31, 2016 to include some things that have been made available since this topic was created, I might as well hit my soap box early on here to talk about the lack of reliability of data that is available in order to determine what disorders are happening.
In a nutshell, it's due to an interplay of those in control of the System not wanting people to figure out just how bad things are which leads to providers being poorly educated, on top of the overall medical industry being in a tailspin of overwhelming redtape and demands, disillusionment, and essentially disruption at this time. The System as we've known it is a house of cards built upon a public that could be kept from being knowledgeable. The Internet changed that. And now, it's potentially collapsing, with the grass roots of other future strongholds having been planted already, which are getting past 'grass roots' at this point in time.
Lewy bodies is always compared to Alzheimer's, which is undeniably the most commonly DIAGNOSED form of dementia. Occurring and diagnosed (and thus into statistics) are two different things. Lewy bodies are referred to in the mainstream article I'll link to and highlight next, and the diagnosable form of it, LBD, is frequently undiagnosed, misdiagnosed ... 'missed'. And it is extremely important people know about LBD.
There are medications which are commonly given to people for some of the symptoms which are helpful for other conditions, which wreak havoc if a person has LBD, so it's VERY important people are aware of LBD. You'll see this repeated in the resources I provide in this topic.
This applies equally to medical providers and consumers; increasingly, the patient or their health advocate/assistant finds information by doing their own research, often online, and provides that to the medical provider/team via email, fax, the mail or in person. Naturally, medical providers also turn to the Interet as well.
From
"Review: management of Parkinson’s disease", found at
www.ncbi.nlm.nih.gov/pmc/articles/PMC3592512/ , (Neuropsychiatr Dis Treat. 2013; 9: 321–340,
Published online 2013 Mar 3), a good 'dot' of information that I think really helps connect those who understand "Parkinson's disease" with "Lewy bodies found in the brain", and thus the 'overlap' with what is then called Lewy bodies disease or Lewy body dementia, or simply Lewy (while many refer to Parkinsons 'Park', for short).
NOTE: I've added additional paragraph breaks for the ease of brains trying to read this information.
Autonomic dysfunctions in PD
Autonomic dysfunction constitutes important constraints in the course of PD. The possible cause are Lewy bodies in brain areas involved in the control of vegetative functions, such as the hypothalamus or the dorsal vagus nucleus, but also in the spinal cord, sympathetic ganglia, and the plexus of the digestive tract.74 The most common autonomic symptoms are orthostatic dizziness, gastrointestinal problems, and bladder and erectile dysfunction.
Concerning orthostatic hypotension and dizziness, nonpharmacological interventions should be attempted first, such as sleeping in a head-up position, fragmentation of meals, avoidance of low sodium and carbohydrate-rich meals, increased water (2–2.5 L/day) and salt intake (>8 g or 150 mmol/L), or wearing support stockings. For medication, fludrocortisone and domperidone might have beneficial effects.75
In contrast, urinary disturbances should be treated primarily with proper medications. These constraints are not only very frequent but also have a severe impact on QOL. Therapeutic options are an optimization of dopaminergic therapy, as this might improve storage properties in PD patients.76,77 However, study results are contradictory.
An alternative might be the prescription of peripherally acting anticholinergics such as trospium chloride (10–20 mg two to three times daily) or oxybutynin (2.5–5 mg twice daily). Nevertheless, there are not enough high-standard studies to assure efficacy.
Other frequent autonomic dysfunctions are gastrointestinal motility problems in PD. Therapy constitutes different approaches: constipation can be treated with macrogol effectively,65 while nausea and/or vomiting in connection with the initial intake of levodopa can be antagonized by domperidone or ondasetron.78
Dysphagia in late stages of PD is also a very disabling and potentially harmful symptom, as malnutrition, dehydration, aspiration, or even asphyxia may occur. Management includes a sufficient dopaminergic therapy, injection of botulinum toxin,79 and different forms of rehabilitative treatments.80
Enteral feeding options such as a short-term nasogastric feeding tube or long-term feeding system (percutaneous endoscopic gastrostomy) can be considered as a final option.
For erectile dysfunction, sildenafil or other phosphodiesterase type 5 inhibitors might be efficacious when considering side effects/contraindications and interactions with other medications.81
The effects of STN-DBS on autonomic symptoms are currently being investigated and, to date, have been considered as investigational. A summary of medical options, their adverse effects, and the level of evidence can be found in Table 5.
The Case Example Inspiring This New Topic at This Time AND My Personal Family History and Learning of Lewy Bodies Disease / Lewy Body Dementia the Hard Way
There are two kinds of people when it comes to learning about this type of information -- those who enjoy a story, examples, and those who don't. If you are one who doesn't, skip over this part.
I turned to the Internet recently when someone I am consulting with/advising about their 'aging' family member, in is needing a 'change of venue' to a more supportive living environment, was the focus of our 1:1 time together (via a mix of telephone and email, and in this person's case, we can work in person as we're physically in the same city, not always the case for those of us who work in distance education with people).
This has been complicated by it requiring changing states, and the family team is wisely not wanting to relinqish the government-assisted housing the person has lived in for a long time if things aren't going to come to fruition in the state they are moving to.
The patient's health advocate got ahold of me mid morning to 'move further along in our process' and inquire about what to do next: their family member, who had been discharged to their care a week prior after a hospital ER admission which lead to a brief (1-2 week) stay at a hospital that specializes in short-term geriatric, psychiatric treatment had been up in the early morning hours having delusions.
I asked what was diagnosed in the end by the psychiatric specialists. What the advocate/family member was told the diagnsosis was didn't mesh with the medications they prescribed. This family member had already 'done her homework' and looked up EVERY medication prescribed and raised questions to the pharmacist they had filled the medications with, and there were some issues they caught but nothing which would cause the type of issues this patient and her 'family system' is experiencing.
Since LBD is so common and so commonly misseDiagnosed, I wanted to be sure that the person wasn't taking something which is contraindicated for Lewy Body Dementia. So that is where I started, was inquiring if any different medications were taken yesterday which might have 'caused the teeter totter to tilt' the direction it went overnight. It's helpful this proactive patient advocate/family member has studied up on the medications since discharge; that is something I had impressed upon them in my iniital 'strategy session' when we all started working together a month before.
This patient may or may not have LBD; that has not yet been revealted but this is an excellent teaching opportunity for ALL who are in similar situations about 'the process'. I 'streamline' things for them by emailing them information so they don't have to sort through unfamiliar territory while they're trying to deal with the realities of having a person with a complex medical condition having difficulties at this moment in their home.
You'll see below that sometimes the onset of the disease is the Parkinson symptoms, sometimes the cognitive/dementia, and sometimes the onset is lead with more of the 'pschiatric' symptoms. Based on what this advocate/family member told me about the facility doing the treatment, it wouldn't surprise me if the facility overlooked considering LBD -- they sounded VERY ineffective. Hence, until I know that someone qualified has ruled out LBD, I'm going to keep it as a possibility to be considering as I assist this medical advocate remotely.
I don't intend to 'call out' any facility in particular in my including this, but to OVERALL remind people that these problems with competence and effectiveness seem to be rampant today. There are ALSO reports of good facilities and good teams and it's a matter of trial and error sometimes. In this case, I have spoken with our area's ombudsman for assisted livings and long term care facilities and found out about another option for psychiatric geriatric hospitialization in our state. I have passed that along to the medical advocate/family member and emailed them the information which follows the line, below.
Figuring if I needed it once, I'll need it again and YOU, another provider or consumer, also can now have the benefit of the resource.
This intelligent, proactive family member had been surprised when a medical provider at the facility 'wanted to talk with her about her language': it wasn't that she'd slipped and used a four letter word,  , the provider was rather condescending about the psychiatric definitions being used. "Did they provide you with a list of terms and educate you?" --- no.
, the provider was rather condescending about the psychiatric definitions being used. "Did they provide you with a list of terms and educate you?" --- no.
So I provided that to her so she could have more confidence in dealing with the hospital staff, because, in my opinion, she was using the medical words appropriately and she was doing a better job of 'diagnosing' the problem than they were. I will set that list up at another topic here in the Forums, so Search on 'psychiatric terms'. It took me a while to find a list I really liked; psychiatry/psychology/mental health is a large part of occupational therapy training from the history of the field but there are few jobs utilizing it today due to the funding changes in the last few decades.
Granted, at that time, they'd only had a few days to work with the patient. But at discharge, which was a 'dump before the weekend deal they did not give adequate preparation time discussing with the family member (because there was a spring break going on with too many staff off then back on, in my opinion), there are discrepancies which indicate how incomplete or inappropriate their treatment was. NOT that we focus on the 'spilled milk', but simply recognizing we have milk to clean up and we need to then have more work on our plates getting things to the right place.
Example: everyone the family member talked to at the facility, as this occurred in summer in Colorado, had just gotten back from vacation and was going off of notes from others, barely having seen the patient.
Had I not had the staggeringly 'mangling medicine' teams related to my father's hospitalization and sub-acute rehabilitation just three years prior, where he was misdiagnosed and missed-diagnosed and hence mistreated for a total of six weeks, the whole way with my saying to each new person I encountered on his medical teams "I don't see that the diagnosis they have given so far accounts for the symptoms, I think he has a progressive neurological disease", which was never acted upon in the facilities, I would not have had the perspective I had with this client.
In my case, things were complicated by the family members/advicates who were present at the time of the acute medical incident and who lived closest geographically were who the medical providers on the team 'honed in on', but they were not in reality related to what the medical problems were in the first place.
They had never had 'the talk' with him about what he wanted and did not want if there were a medical incident; I had, just three months before when they were out of the country and I was in charge. I was going to insist we get things 'grouped up' the day after the next holiday, and the medical event occurred a few days prior to that. The good thing is, I was on a 'wild ride' like this patient is, something I would not have ever experienced had it all been left up to me, and now I have a much bigger 'fund of knowledge' about how badly a medical team can ignore information coming from even medically qualified family members and how many things can go wrong.
Again, not "crying over spilled milk", but really suggesting to families to MAKE THE TIME to do proper planning, you'll be saving yourselves a TON of time and 'dramedy' if you do. "I should have made the time" this family member advocate said. I replied "If you learn how to 'make time' please let me know." Sometimes there is nowhere to sqeeze time for people; jobs/work, dependent children, spouses, houses and aging family members.
That is when a professional advocate/advisor/assistant can come to the rescue! I've been told even in the beginning 'strategy session' that what I was doing was extremely valuable to this already-busy family member who was volunteering to help 'the family team' out by also putting this on her plate. I even check in and try to be supportive and give a little laugh -- that's so key to getting through these situations.
"I'm sorry this is happening to you; it has happened to me too. We're in this together and we'll get through it, let's just do our next step and that should be....." ..... And in this case with my client, it was to provide education about Lewy Bodies Dementia/Disease. (In the end, this client said that of all the people they know via their professional and personal circles, my advise was the most overall helpful -- an unsolicited 'endorsement statement' I thought I'd sprinkle in here.)
In my father's case, a home health nurse -- yes, he had to get all the way home and a nurse said the same thing I'd been saying for a LONG time, and finally those who needed to accept it 'were receptive' and in four more months there was finally a diagnosis and complete treatment of LBD, which was enormously helpful in his case! (Nurses, like occupational therapists cannot 'diagnose' things, we operate off of the diagnosis of medical providers who are deemed more qualified than we are, but on GOOD medical teams, they will take in the information of the other medical professionals and family, for that matter).
Please go to the website for the LBDAssociation (link below), and look around beyond this one topic. There are also other organizations, I like one out of the UK a lot as well. The Alzheimer's Association also includes some information but I shy away from directing people that direction ONLY because they are NOT the same disease and LBD will continue to get shoved under the rug and be unknown and underdiagnosed if it's not seen in it's own 'right'. If the two groups would merge and create something like 'The Dementia Society', that would be ideal. Dr Lewy and Dr Alzheimer were colleagues and one discovered one thing and the other another, which is so interesting that it's taken the journey it has. Again, the business world, the nonprofit organization world, the medical world -- the overall world, is not perfect. But we are in this together and we'll get out of it together if we all get in the right frame of mind. Just like this client and I and her family member's team will.
PS -- I just looked at the date of when this 10 Things You Should Know about LBD was created at the LBDA.org website. Interesting 'coincidence' -- on that day, the hospital which totally missed (intentionally or accidentally) any movement disorder (even a Parkinson's diagnosis) and had put in an unnecessary feeding tube instead of prescribing a simple medication and swallow/speech therapy (and PT/OT) was being paid by his insurance on that day for his 'care'.
Suffice it to say, this has recommitted and reminded me of this ongoing 'fight' we all have with the medical system around us. I hope this topic is informative and that my experience and training can assist you if you're reading or need individual consultation and advise. And for what it's worth, I'd never had a patient diagnosed with LBD -- I often had patients go to their doctor because they presented seemingly to have Parkinsons with an interesting form of difficulty with complex thinking that didn't seem quite like dementia to me.
I actually told other medical providers "it's like there's something that has not been discovered yet". It HAD been discovered, long ago, but none of the doctors I worked under orders from apparently were aware and diagnosing it. I saw balance problems and cognitive problems for complex issues in 1996 when he was in his mid 70s and started intervening and he refused to seek medical advise. Changes in 'complex thinking' such as how to problem solve a dead battery or change out a sink came to light about five years later and it was 2009 when he was finally diagnosed. It took 'all the wagons to get in a circle' -- the WHOLE family team has to get on board WITH the medical team in order for a medical situaiton to be handled 'ideally' in terms of "efficient" and "effective". I would be remiss if I did not underscore that, above. The patient 'suffers' if not. And isn't that who we are serving/advocating for/working for, our customers/patients/loved ones?
10 Things You Should Know about LBD
12/31/2008
Lewy body dementias (LBD) affect an estimated 1.3 million individuals and their families in the United States. At the Lewy Body Dementia Association (LBDA), we understand that though many families are affected by this disease, few individuals and medical professionals are aware of the symptoms, diagnostic criteria, or even that LBD exists. There are important facts about Lewy body dementias that you should know if you, a loved one, or a patient you are treating may have LBD.
- Lewy body dementias (LBD) are the second most common form of degenerative dementia and is widely under-diagnosed: The only other form of degenerative dementia that is more common than LBD is Alzheimer’s disease (AD). Many individuals who have LBD are misdiagnosed, most commonly with Alzheimer’s disease if they present with a memory disorder or Parkinson’s disease if they present with movement problems.
- LBD can have three common presentations: Some individuals will start out with a movement disorder leading to the diagnosis of Parkinson's disease and later develop dementia. Another group of individuals will start out with a memory disorder that may look like AD, but over time two or more distinctive features become apparent leading to the diagnosis of ‘dementia with Lewy bodies’ (DLB). Lastly, a small group will first present with neuropsychiatric symptoms, which can include hallucinations, behavioral problems, and difficulty with complex mental activities, leading to an initial diagnosis of DLB. Regardless of the initial symptom, over time all three presentations of LBD will develop very similar cognitive, physical, sleep and behavioral features, all caused by the presence of Lewy bodies throughout the brain.
- The most common symptoms of LBD include:
Dementia: problems with memory and thinking
Hallucinations: seeing or hearing things that are not really present
Cognitive fluctuations: unpredictable changes in concentration and attention
Parkinson-like symptoms: rigidity or stiffness, shuffling gait, tremor, slowness of movement (bradykinesia)
Severe sensitivity to neuroleptics (medications used to treat hallucinations)
REM Sleep Behavior Disorder: a sleep disorder where people seemingly act out their dreams
- The symptoms of LBD are treatable: Currently there are no medications approved specifically for the treatment of LBD. All medications prescribed for LBD are approved for a course of treatment for symptoms related to other diseases such as Alzheimer’s disease and Parkinson’s disease with dementia and offer symptomatic benefits for cognitive, movement and behavioral problems.
- Early and accurate diagnosis of LBD is essential: Early and accurate diagnosis is important because LBD patients may react to certain medications differently than AD or PD patients. A variety of drugs, including anticholinergics and some antiparkinsonian medications, can worsen LBD symptoms. LBDA has compiled a list of medications that should be avoided.
- Traditional antipsychotic medications may be contraindicated for individuals living with LBD: Many traditional antipsychotic medications (for example, Haldol, Mellaril) are commonly prescribed for individuals with Alzheimer’s disease and other forms of dementia to control behavioral symptoms. However, LBD affects an individual’s brain differently than other dementias. As a result, these medications can cause a severe worsening of movement and a potentially fatal condition known as neuroleptic malignant syndrome (NMS). NMS causes severe fever, muscle rigidity and breakdown that can lead to kidney failure.
- Early recognition, diagnosis and treatment of LBD can improve the patients’ quality of life: LBD may affect an individual’s cognitive abilities, motor functions, and/or ability to complete activities of daily living. Treatment should always be monitored by your physician(s) and may include: prescriptive and other therapies, exercise, diet, sleep habits, changes in behavior and daily routines.
- Individuals and families living with LBD should not have to face this disease alone: LBD affects every aspect of a person – their mood, the way they think, and the way they move. LBD patients and families will need considerable resources and assistance from healthcare professionals and agencies. The combination of cognitive, motor and behavioral symptoms creates a highly challenging set of demands for continuing care. LBDA was formed to help families address many of these challenges.
- Physician education is urgently needed: An increasing number of general practitioners, neurologists, and other medical professionals are beginning to learn to recognize and differentiate the symptoms of LBD from other diseases. However, more education on the diagnosis and treatment of LBD is essential.
- More research is urgently needed! Research needs include tools for early diagnosis, such as screening questionnaires, biomarkers, neuroimaging techniques, and more effective therapies. With further research, LBD may ultimately be treated and prevented through early detection and neuroprotective interventions. Currently, there is no specific test to diagnose LBD.
THIS INFO WAS AT ANOTHER LINK AT THE LBDA.ORG WEBSITE, FYI. Again PLEASE follow the link to the website to get the 'full effect', there are just the highlights to encourage you to know it's a GRATE site to visit!
End-of-Life
Planning for the end of life can be a valuable activity for any family. The links below offer general guidance and some specific suggestions for families who face the burden of a disease such as Lewy body dementia.
Advanced Directives - a Caring Connections site with state-specific advanced directives
Caring Connections - home page of consumer Web site about hospice and palliative care managed by the National Hospice and Palliative Care Organization
Palliative Doctors - a Web site for consumers managed by the American Academy of Hospice and Palliative Care about palliative care
Editing 3/31/2016 - 1,160 reads at this point. It came up in conversation with someone who I suspect has possibly been underdiagnosed at this point, that orthostatic hypotension is something to consider.
I related to this person my experience of fourty years ago, when I was a teenager and would grey or black out virtually every time I went from sit to stand, all day long -- at home, at school, on the school bus ..... which made me more 'aware' and 'empathetic' about others ever since.
I spend a lot of time on Facebook, since 2008, building connections and getting into groups which show up in my feed that remind me of the various health issues I keep up on. These disorders that we think of as separate are really overlapping and most everyone has symptoms of them. As people are with more exposures over time, you'll see the symptoms getting worse, but when you are a medical detective 'onion peeler' like I became in the last decade or two, it becomes clearer with every case you work with.
What prompted the conversation was an immediate concern about controlling edema in the lower extremities. The nemesis of my days working as an occupational therapist was 'those darn compression stockings' (back then called TED hose). I joked that I used to tell people they were nemesis socks. It wasn't so bad when it was someone who was going to reside in long-term care or even assisted living -- they could have assistance donning and doffing them (taking them on and off).
There are gadgets out there which insurance typically paid for, and OTs would get into the hands of patients in the hospital typically, or in subacute or acute rehabilitation, that I'd then write goals for and work with those patients on and typically we'd give up on it and resign ourselves to that assistance would be given for the 'darned things'.
I had a patient along the way in my years working skilled nursing in Denver, Colorado Springs and finally Grand Junction, Colorado, who'd been a high level nursing manager at a hospital prior to her reaching the age she'd retire. She had no family to assist locally, but had her cognition in tact. She had thoughtfully packed her bags to go to the hospital for a scheduled hip replacement surgery, knowing she'd go on from there to skilled nursing for sub-acute rehabilitation and THEN home -- she had everything she'd need.
And somehow she would manage, starting in the wee hours of the morning, to put on the prescribed compression stockings independently using assistive devices -- in her case, unbelievably, her reacher, not the 'sock aid'. If I recall correctly, it took about an hour. Keep in mind, after hip replacement you're ordered to not bend at the hip past a certain point. My mind was blown.
It was also blown when we went to do her home assessment when she was ready for discharge to home -- there was no way a walker could be used in the home because of all the items she had in the home. There wasn't a single seating surface to sit on, nor a place on the stove top to set anything. This was before we had the term 'hoarder' in our vocabulary. And what was the most interesting to me was she'd prepared her bags so precisely but hadn't known we'd do a home assessment, since her experience was at the hospital level as a nurse and they don't do home assessments.
This was the patient who inspired me to go track down the facility psychologist and ask him why a person would hold onto a hazardous amount of things. "Everyone has to have an outlet in some way for upsetting things" was his response. I said "I thought it would be more in the realm of obsessive / compuslive ...." and he said "that's what a psychiatrist would say, and then they'd prescribe a medication." So how many professionals does a person have to have on their team in order to get advise and solve their problems? This one had doctors, nurses, PT, OT and now is needing both psychologist and psychiatrist?
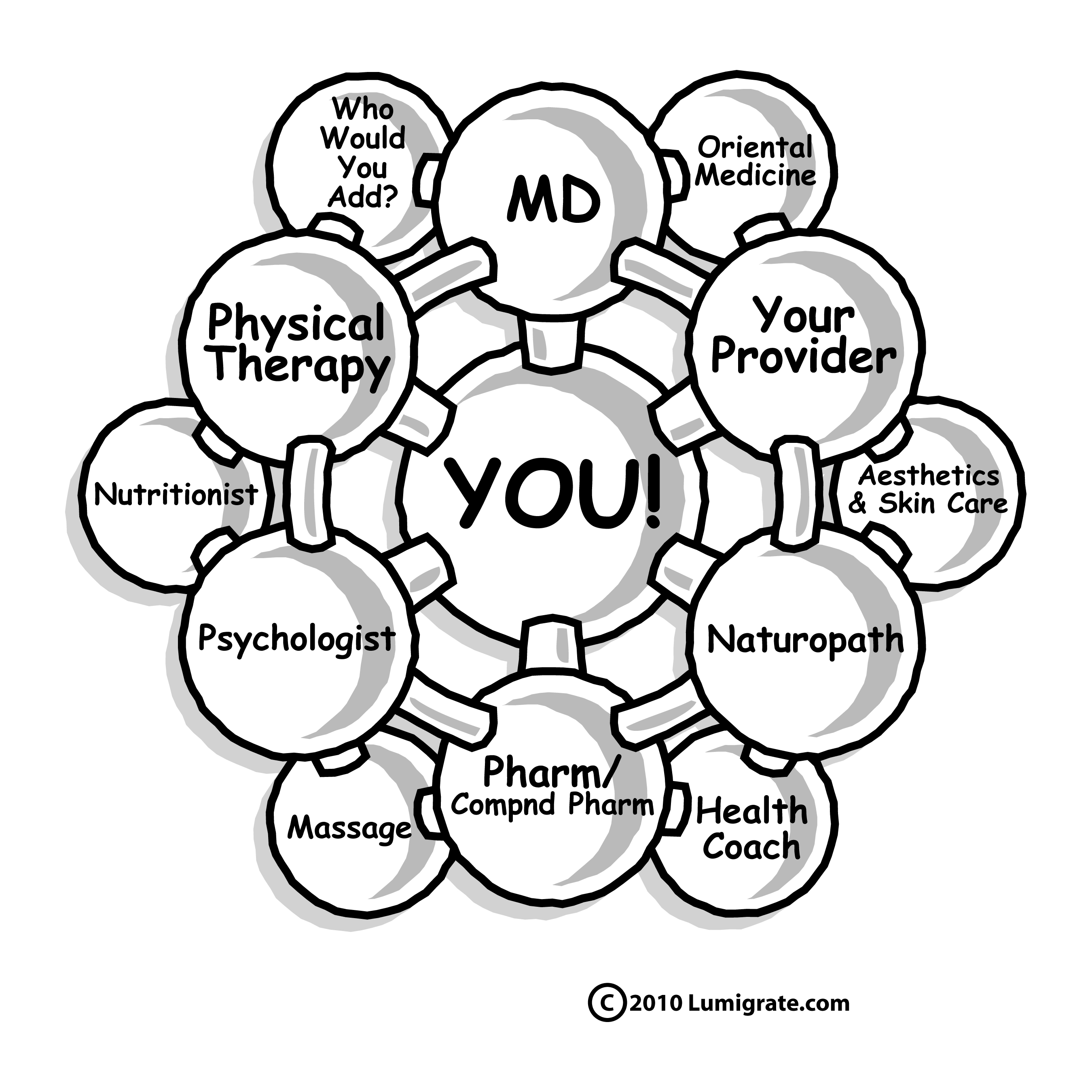
The Lumigrate YOU! Model would later be born with the help of another psychologist, a pain management - neuro-focused psychologist in Grand Junction, who I collaborated well with for the three years (early 2005 to early 2008) - the model was brainstormed in one of our meetings, at my request, based on a rheumatologist's request of me to have a group for patients with chronic fatigue and pain, as she mapped out all the types of providers over the course of a year and ongoing, these patients could MOST BENEFIT FROM. "There's little I can do for them, they really need PT, OT, psychology primarily, and keeping up with endocrinology, neurology and rheumatology as well as their primary care provider, naturally."
Part 5, YouTube channel LBDAtv (so go to the search bar at YouTube, look for LBDAtv as a channel, you'll see much more than just this one thing, and perhaps something else will be the better starting point for YOU. But I suggesting finding this five part series, titled
"Difficulties in Diagnosing Lewy Body Dementia". Parts 1-4 are good to watch as well, I chose to type out the highlights of part 5 for our YOUsers
Summary
LBD is the second or third most common cause of dementia.
Presents with
- Alzheimer-like dementia
- Mild Parkinsonism
- Prominent hallucinations
- Severe reaction to neuroleptics - Inappropriate treatment of the psychotic symptoms can have severe consequences, therefore it's very important to consider LBD as a diagnosis. You want to be open minded. You don't want to be like HM Warner who owned Warner Brother's Studio, who said 'who wants to see actors talk'.
Medications for Cognitive Impairment / "Dementia":
There's a lot of false hope when it comes to what the medications will do, in his opinion. He goes on a rant about pharmaceutical companies marketing to the consumer and how the consumers expect medications as a result. Medications for dementia will typically reverse symptoms by up to a year in most cases, but it's not neuroprotective and then the symptoms continue to advance.
However, there are gastrointestinal side effects, and thus weight loss (20% lose weight), which becomes one of the bigger concerns. You don't want people getting frail -- PEG tubes, no padding/fat and breaking hips with falls, or skin breakdown from the nutrition deficiency. So he skips treating with the medications, typically.
PT / OT (though he does NOT mention occupational therapy but that is who typically will get into the assistive devices beyond what PT focuses on -- to have PT without OT ALMOST ALWAYS leaves a gap, as they are a 1-2 punch / team in most environments, BUT for various reasons (incompetence being one, shortages of staff being another, cost saving by agencies another .....) PT is sometimes the only order written and the PT doesn't request OT. I saw it over and over again when working in outpatient and home health).
Physical therapy, home visits -- assistice devices, attention to environmental safety to minimize fall risk is the 'best bang for your buck', he states.
The Overlap with CardioVascular, Blood Pressure, Edema
A lot of walking keeps the blood vessels working, and the muscles ......
Consuming a lot of fluid. The osmostat in the brain doesn't work; "Older people never drink enough"
Salt. People over 60 learn "salt is poison." Unless you have CHF or kidney failure, you don't need a sodium restriction. And even if you do .... hypertension, heart attack and dying is probably not as bad as breaking a hip and what all you deal with for time after that, I'm going to be real blunt about it. ... We use a lot of salt."
(Mardy's note: I hope people will investigate the types of salt and what type they believe is best. Table salt. Iodized salt. Sea salt. Ancient sea salt (which I personally prefer, and can be obtained much cheaper than the Himalayan brands. One needs to check into how the salt is extracted from the Earth because some places just blow it up with things that will leave traces of heavy metals in the salt you consume...... ). Within something as simple as salt, or water, there are enormous amounts of information to sift through eventually for learners.... )
The most common drug prescribed by a leading expert on orthostatic hypotension he refers to: "salt tablets". (Again, see the allopathic approach to this, prescribing tablets of salt versus having people get the salt from 'outside the system' of insurance-based medicine. Sometimes this can be a good starting point to use what is prescribed by allopaths and then transitioning .... )
Intestinal Wellness / Elimination / Constipation
Bowel hygiene - Walking. Fluids. Diet. Add Flax Seed, or Uncle Sam Cereal. "We'll add in colace or other stool softener, then something like Senicot or then Lactulose or Sorbitol -- we do whatever is necessary, these people do get constipated." (Mardy's note, I'm spelling these from memory, don't quote me on spellings....)
Mardy's note: This is a very allopathically-oriented presenter, I encourage people to learn what providers 'outside the box' would suggest. Sometimes when a person has been immersed as a consumer in allopathy (and their support team helping them at home), it's a good starting point to go with the allopathic products even if insurance doesn't pay for them or you have a big copayment, then work with providers who will help you transition to more commonly available or natural versions. They're typically less costly as well, though you might need to pay in the beginning for the provider (since they can't be reimbursed by The System / insurance.)
And interestingly, there's 'overlap' from what I'm aware of what naturopathic doctors or colon hydrotherapists would suggest, in the flax seed / fiber aspect. NDs and CHs sell products out of their offices to help with the overhead costs and to have things readily available for their patients / clients to purchase, and they also typically will be aware and suggest shopping on the Internet. Let Amazon be your friend, as the saying goes.
Management of psychotic symptoms -
"....you have to be gentle about this. .... There's a stigma about mental illness. Our favorite is benign neglect" he says. He goes on to relate how it's difficult for families sometimes, as it'll be the family patriarch / matriarch who is having hallucinations. (Benign neglect means not treating.) Or low dose of some medications, listen to the presentation if interested in details. The first question is 'do you HAVE to do something' and typically you don't -- awareness of the family and patient is helpful. The emotional reaction to the hallucination improves. They're not calling the cops when seeing someone there, etc.
"Having people around seems to reduce hallucinations." When people move into facilities or with family, they reduce or go away.
Mardy's Note: I recall one of my first multi-week motorcycle trips with my to-be second husband driving, around the Southwest of the US from our home in Fort Collins, Colorado in my mid 20s. The motorcycle was an old BMW with a radio he could hear but not back where I was.
This was to be replaced after that trip due to the engine going out with a used by much newer Yamaha with fancy helmets and headsets with sound and microphones. Somewhere in the second week of not having music on the radio in the house, the car -- which was my normal everyday life my whole life to that point, I started being able to do a jukebox in my head.
I could think of any song title and it would come up and I could hear it as if it were playing on a device! I wonder if this was an early symptom for me, or if this is the signs of a healthy brain when it's bored --- riding on the back of a motorcycle is not the most entertaining thing, leaving you a lot of time for thought and .... hearing music in your head.
I've been seeing various common traits in people who have these movement disorders, and one thing I've noticed is an ability to seem content with far less interaction with other people than 'the norms of society', to be considered even reclusive. Just an observation and comment 'for what it's worth' to YOUsers reading this topic. ~ Mardy
The emotional reaction to the hallucinations gets better as well, with treatment and recognition of the team that the hallucinations are simply part of this disorder.
Abilify is new medication which they avoid, it's caused problems with Parkinsons motor symptoms.
"You don't treat anything until you diagnose it." he reminds. And then summarizes as he wraps it up:
This is a common illness. It causes a lot of difficulties. You can improve it a lot with management. If you don't look for the symptoms of Lewy body and you get the wrong medication, you can get in big trouble. Be open minded -- don't see everything as a subtle variance of Alzheimer's disease. Move forward with the times.
Live and Learn. Learn and Live Better! is my motto. I'm Mardy Ross, and I founded Lumigrate in 2008 after a career as an occupational therapist with a background in health education and environmental research program administration. Today I function as the desk clerk for short questions people have, as well as 'concierge' services offered for those who want a thorough exploration of their health history and direction to resources likely to progress their health according to their goals. Contact Us comes to me, so please do if you have questions or comments. Lumigrate is "Lighting the Path to Health and Well-Being" for increasing numbers of people. Follow us on social networking sites such as: Twitter: http://twitter.com/lumigrate and Facebook. (There is my personal page and several Lumigrate pages. For those interested in "groovy" local education and networking for those uniquely talented LumiGRATE experts located in my own back yard, "LumiGRATE Groove of the Grand Valley" is a Facebook page to join. (Many who have joined are beyond our area but like to see the Groovy information! We not only have FUN, we are learning about other providers we can be referring patients to and 'wearing a groove' to each other's doors -- or websites/home offices!) By covering some of the things we do, including case examples, it reinforces the concepts at Lumigrate.com as well as making YOU feel that you're part of a community. Which you ARE at Lumigrate!
This forum is provided to allow members of Lumigrate to share information and ideas. Any recommendations made by forum members regarding medical treatments, medications, or procedures are not endorsed by Lumigrate or practitioners who serve as Lumigrate's medical experts.


![Expand cart block. []](/sites/all/modules/ubercart/uc_cart/images/bullet-arrow-up.gif)

